- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (718)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
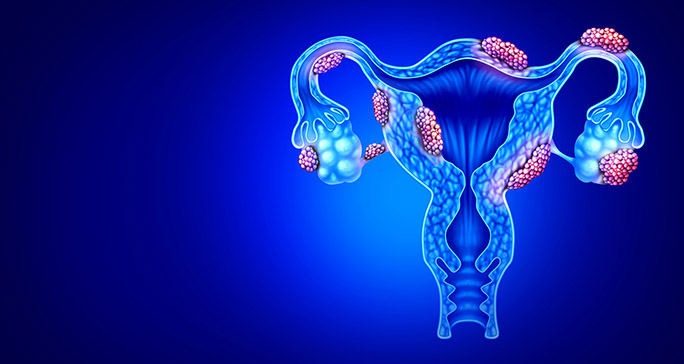
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (164)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (124)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (898)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1776)
How molecular testing and targeted therapy are changing B-cell lymphoma treatment
BY Devon Carter
4 minute read | Published November 18, 2020
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on November 18, 2020
B-cell lymphoma isn’t one disease. There are about 63 subtypes, with diffuse large B-cell lymphoma (DLBCL) being the most common. A chemotherapy regimen called R-CHOP has been the standard treatment approach since 2002, when the antibody therapy rituximab was added to the chemotherapy regimen CHOP.
Almost 60% of patients find success with R-CHOP. But what about the remaining 40% of B-cell lymphoma patients?
“The success of treatment really depends on which subtype you have,” says Christopher Flowers, M.D., co-leader of MD Anderson’s B-Cell Lymphoma Moon Shot®.
Molecular testing offers an accurate diagnosis, tailored treatment for B-cell lymphoma
Because so many patients see success with chemotherapy, B-cell lymphoma is commonly thought of as one of the most curable cancers. But Flowers cautions that’s not true for every patient.
“We now have molecular tests that identify different subgroups of B-cell lymphoma patients,” Flowers says. “So we know some patients have an 80% chance of a cure with R-CHOP, but in that same pool, we’ll find others who we have about a 30% chance.”
Molecular testing identifies a cancer’s unique cellular qualities. This insight enables doctors to treat a patient’s specific cancer more precisely.
To ensure that you’re receiving the best treatment for your exact B-cell lymphoma diagnosis, it’s best to seek care at a specialty cancer center like MD Anderson from the beginning, advises Flowers. That way, you can get molecular testing before starting treatment.
“Molecular testing isn’t done out in the community. That means in many cases, B-cell lymphoma is treated as one disease with one treatment plan,” Flowers says.
At MD Anderson, patients receive testing to identify their subtype, which then informs decisions about their treatment. The process involves experts in pathology and cancer medicine. “That way, we can better predict how a patient will do with chemotherapy and offer what may be a more effective approach,” Flowers says. In many cases, he says, patients are offered one of MD Anderson’s nearly 100 B-cell lymphoma clinical trials, giving them access to the most cutting-edge approaches to treatment.
Improving molecular testing for B-cell lymphoma
To receive molecular testing, patients have traditionally had tissue surgically removed from a tumor and sent a lab.
But researchers led by Michael Green, Ph.D., are developing a liquid biopsy to improve the process of undergoing molecular testing. “We’re working on something called cell-free DNA, where we can see the DNA of the tumor circulating in a blood sample,” Flowers says. This will allow patients to avoid the traditional approach of a surgical biopsy.
Avoiding chemotherapy with targeted therapy
After molecular testing, we know the unique markers of a cancer, enabling doctors to more accurately treat it with an approach called targeted therapy. Sometimes called precision medicine, targeted therapy aims to match the right patient with the right treatment at the right time. Targeted therapies home in on specific cells that fuel a cancer’s growth and slow or stop them. Because targeted therapy is so exact, patients typically have fewer side effects.
In a first-of-its kind approach, the Smart Start Clinical Trial led by Jason Westin, M.D., offered newly diagnosed diffuse large B-cell lymphoma patients a combination of the targeted therapies ibrutinib and lenalidomide without chemotherapy first, and followed by the combination given with the standard R-CHOP regimen.
“What we learned on Smart Start was that the targeted treatments work really well for patients with DLBCL,” Westin says. The overall response rate was 86% prior to patients receiving any chemotherapy. 50% of patients had a partial response. “This is not a trivial finding,” Westin says.
“With these results, we think there may eventually be some patients who we can identify who don't need chemotherapy at all,” Flowers adds.
Westin is working to build on the success of the Smart Start clinical trial with a new study that will test the targeted approach with a new combination of lenalidomide, acalabrutinib and tafasitamab. The study will also extend the treatment course from two cycles of the targeted therapies to four cycles. Westin says the goal is to increase the number of patients seeing their cancer disappear with the targeted therapies alone.
“This trial is one in a million. But if we don't try, then we're going be stuck in the 1970s,” Westin says. “And nobody else is doing anything like this.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Related Cancerwise Stories

The success of treatment really depends on which subtype you have.
Christopher Flowers, M.D.
Physician