- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (294)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (892)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1772)
How interventional radiology is used to manage cancer-related bone pain
BY Devon Carter
5 minute read | Published January 04, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 04, 2022
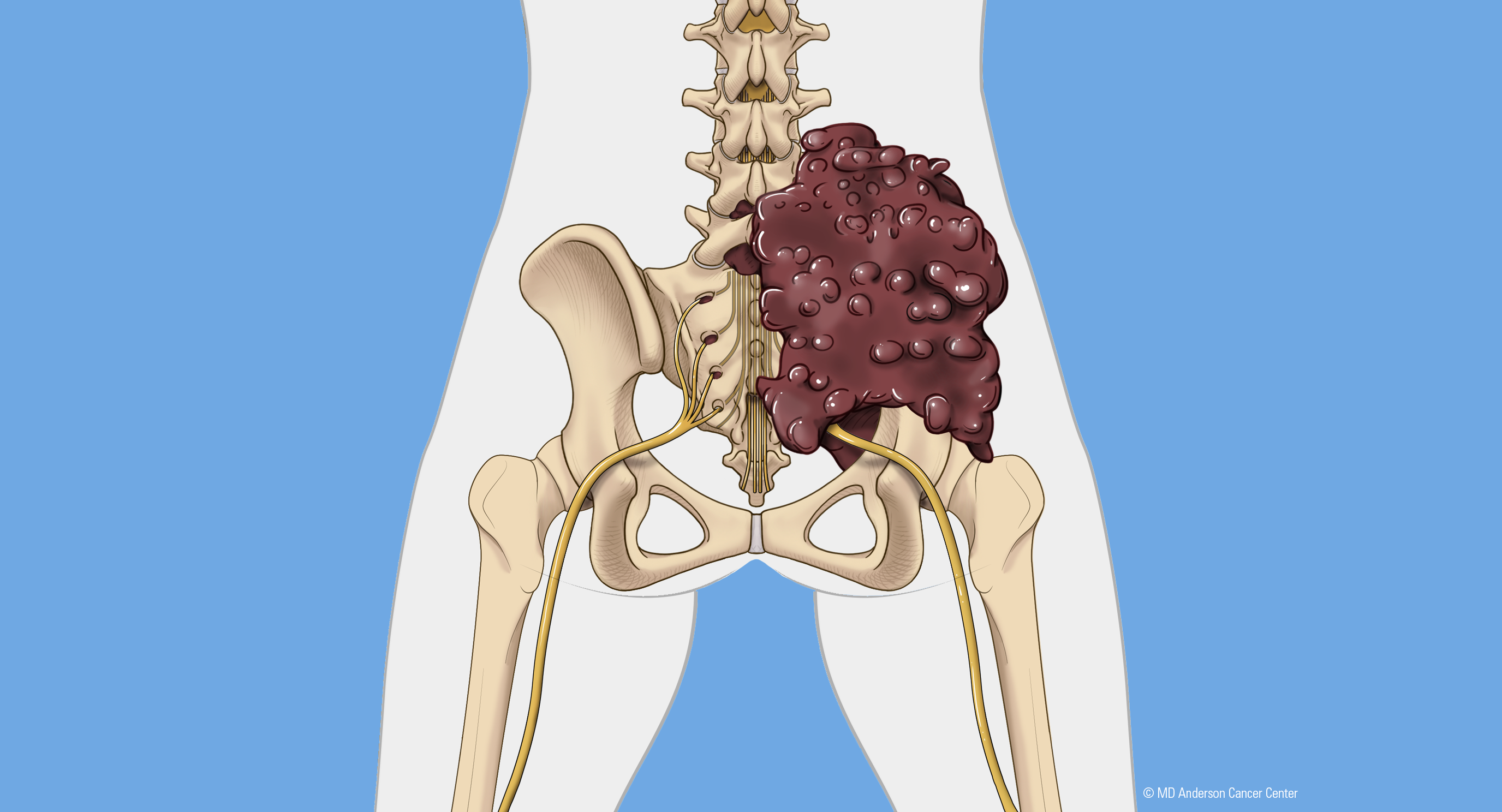
Many types of cancers can spread to the bone, leading to areas of damage called lesions. 80% of patients with metastatic prostate cancer develop bone lesions, but it’s also common in patients with many other types of cancer including metastatic breast cancer and metastatic renal cell carcinoma. These lesions leave patients in pain and sometimes impact mobility. They’re most commonly found in the ribs, the pelvis and the spine. Bone metastases occasionally occur in the shoulders and legs.
Usually, chemotherapy or immunotherapy can treat a bone lesion, and radiation therapy and pain medicine help manage their associated cancer pain. But these traditional methods don’t always work or aren’t an option for all patients.
MD Anderson is leading a new approach for patients with bone metastases that uses interventional radiology. These techniques offer patients a new option for pain management that can provide fast relief with few side effects. Interventional radiologist Rahul Sheth, M.D., shares how these minimally invasive procedures are changing the way we manage cancer bone pain.
What is interventional radiology?
Interventional radiology combines diagnostic imaging techniques like X-rays or CT scans with therapeutic procedures done inside the body. The procedures are performed through small pinholes in the skin and can help address a variety of medical concerns – not just cancer. The diagnostic imaging tools allow us to take pictures in real-time during the procedure. That way, we know exactly where everything is at all times without having to make a big incision to open the patient up.
Instead, patients receive small punctures, similar to needles through the skin. And, there are no stitches afterward. We essentially put a Band-Aid on top while the punctures heal over the next couple of days.
For patients with bone metastases, interventional radiology can provide a real benefit in managing pain. Although each patient is different, most people go home the same day or the next day, and they feel relief a few days after the procedure.
Reasons for cancer bone pain
Bone tumor-related pain can be caused by one or a combination of three things. The first is the cancer cells themselves. When the tumor’s cells take root inside the bone, their presence releases inflammatory proteins, which cause local inflammation. The brain perceives that inflammation as pain.
Second, as the cancer cells erode the bone, they can cause inflammation at the lining of the bone, which is where nerve fibers are found. As the tumor grows and the lining of the bone stretches, and the tumor can break out of the bone and cause pain.
Lastly, if the tumor is on a weight-bearing bone like the spine or the pelvis, it can cause pain. It’s just like when you break your wrist: There are fractures in the bone, and the fragments move around. As you move, the fragments rub against each other and can’t heal. This leads to inflammation that causes pain.
With interventional radiology, we tailor our treatment approach to address which of these three – or all three – are causing the pain.
When pain medicine and radiation therapy aren’t an option, interventional radiology may be
Even when prescribed at a high dosage, an opioid may not relieve bone cancer pain for a patient. Interventional radiology procedures can help wean patients off opioids while offering long-term pain relief.
Radiation therapy is another common approach for addressing pain, but it’s not an option for everyone. If a patient has already received radiation in that area, this treatment can’t typically be used again. But another benefit of interventional radiology is that the procedures can be repeated. Also, if a patient is receiving chemotherapy, they may have to pause the drugs to schedule radiation therapy. If the cancer is aggressive, this could be an issue. Interventional radiology is conveniently combined with other treatments since the procedures and recovery are quick.
Some cancer types are known to be resistant to radiation therapy. In those cases, we try to be more aggressive with treatment. At MD Anderson, we’re conducting a clinical trial that’s investigating stereotactic body radiation therapy combined with interventional radiology techniques. Our goal is to speed up how soon patients feel relief and maximize how long that relief lasts.
Interventional radiology helps destroy a bone tumor
The best way to address pain directly caused by a tumor on the bone is to eliminate the tumor. Two interventional radiology approaches we commonly use are ablation and embolization.
- Ablation: We destroy a tumor by subjecting it to extreme temperatures – either hot or cold. We insert a needle through the skin and into the tumor. That needle generates heat at its tip to heat the tumor, or it freezes the tumor into a ball of ice. We monitor the size of the ice ball with imaging techniques. This allows us to ensure we’re treating the entire tumor and avoiding surrounding normal tissue. At MD Anderson, we’re also exploring using ablation to improve systemic cancer treatments like immunotherapy.
- Embolization: By working with a patient’s blood vessels, we can destroy a tumor. Like the way cardiologists place stents in the blood vessels supplying blood to the heart, we do the same thing to the blood vessels supplying blood to a tumor. We enter the body, often through the leg or the wrist, and navigate to the tumor inch by inch, using X-rays to follow along. Next, we pack the blood vessels with thousands of microscopic plastic beads that float deep into the tumor and block the blood flow. This cuts off oxygen and nutrients and leads to the tumor’s death.
We often combine these techniques to maximize their benefit.
Bone cement stabilizes the bone to relieve pain
If the pain is caused by a tumor destroying the bone, we have a different approach. Much like a cast helps hold together broken bone so that it can heal, we do the same thing on the inside with bone cement. We glue together the bone fragments to hold them in place and speed up healing. The cement stops the constant motion of the fractured bone, and the patient feels relief soon after the procedure. In our recovery area, patients often already start to feel improvement in their pain levels.
This pain is a huge quality of life factor for our patients, and it’s gone within a few hours, thanks to these approaches. Personally, it's very fulfilling and rewarding work.
Request an appointment at MD Anderson online or by calling 1-844-929-4217.

Our goal is to speed up how soon patients feel relief and maximize how long that relief lasts.
Rahul Sheth, M.D.
Physician