- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (918)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (182)
- Treatment (1786)
Using my experience with colorectal cancer, Lynch syndrome to help others
5 minute read | Published May 05, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on May 05, 2021
In 2016, my daughter was six months old, and I was still working on recovering from a difficult pregnancy. I had gone back to work as a special education administrator and was juggling a lot of responsibilities. I started having stomach issues, but I assumed it was an ulcer based on my previous experiences. I was only 32 at the time and chalked it up to the stress of being a new mom.
My stomach issues started off as a dull ache. Sometimes, I felt full soon after beginning to eat. I went to an urgent care facility and, after describing my symptoms, was sent home with anti-nausea medication.
A week later, I was constantly nauseous and vomiting. I ended up in the emergency room, where the doctor ordered a CT scan.
When the doctor returned to my room with the results, I knew something was wrong. He diagnosed me with stage IV colorectal cancer and told me to get my affairs in order. I had a grapefruit-sized tumor on my colon and metastatic growths on my liver.
I was shocked. I was young, healthy, and of the many ultrasounds done during my pregnancy, none had showed anything suspicious. Being a brand-new mom, I was not ready to give up. I wanted a second opinion – and a chance to fight.
Genetic testing reveals Lynch syndrome diagnosis
After being discharged from the hospital, I began to research my treatment options. My husband helped me to request an appointment at MD Anderson through the online form, but before I could even meet my care team, I was admitted to the emergency room at MD Anderson due to a bowel obstruction. Since the nausea was not allowing me to keep food down, I underwent surgery to place a temporary ileostomy. This diverted my small bowel to an artificial opening on my abdomen to collect waste.
My oncologist Dr. Bryan Kee worked with the rest of my care team to develop my treatment plan. Within one month, I began seven rounds of a combination chemotherapy regimen, including fluorouracil, oxalitplatin and irinotecan.
When I started chemotherapy, I also met with MD Anderson fertility specialists. Because chemotherapy can hamper fertility, I took medication to stall my ovarian function in the hopes that some eggs could be saved. Blood testing showed I still had good hormone levels and some eggs remaining after treatment.
I also underwent genetic testing. That’s how I learned that I had Lynch syndrome, which significantly raises a carrier’s risk for developing colorectal, endometrial and other cancers. Because Lynch syndrome can make cancer more aggressive, Dr. Kee added an additional chemotherapy drug, bevacizumab, to my regimen.
After I was diagnosed with Lynch syndrome, my care team expanded exponentially. Dr. Denise Nebgen became my gynecologist. I see her for biopsies and an ultrasound once a year. Dr. Nebgen and I have also discussed preventive surgery to reduce my risk of developing other cancers. After I turn 45 years old, I will undergo a hysterectomy to remove my uterus and ovaries.
My surgery and immunotherapy treatments
Following chemotherapy, I underwent another surgery to reverse the ileostomy, and Dr. Brian Bednarski took out all of the tumor on my colon. The cancer was also in my lymph nodes, but they couldn’t be safely removed, due to their location close to a large artery.
After surgery, I qualified for immunotherapy because of my Lynch syndrome. I started 34 cycles of the immunotherapy drug pembrolizumab in April 2017. Two years later, I completed immunotherapy, and I have showed no evidence of disease since then.
Dr. Kee and his whole team have stood by me from the beginning. The nurse advanced practice providers are wonderful, and there are so many others who have helped me. Understanding the importance of my faith during cancer treatment, MD Anderson even made sure my spiritual needs were met. They offered both mental health help and spiritual health help, enabling me to see both a chaplain and a psychologist. They gave me the tools to make sure all parts of myself were recovered and healed after treatment.
MD Anderson is a huge hospital, but they have someone to help you with everything you can think of. They take care of the whole person, not just the part of you with cancer. And everyone cares. It’s unlike any hospital I’ve ever been to.
Look for ‘future you’
During my immunotherapy treatment, I lost a friend who had been going through cancer treatment at the same time I was. When she passed away, I went through survivor’s guilt. It is so isolating. But I knew she would have wanted me to help other people by sharing our stories. I try to emulate her by focusing my energy on having a positive attitude. It doesn’t heal you, but it helps you get through the tough times.
When people ask about my experience or how they can be there for a friend going through cancer, I always tell them not to be afraid to be there. Talking about cancer can make people feel uncomfortable, but don’t stop reaching out to someone who may need it.
During my treatment, I had an amazing support system, but I know that’s not true of everyone facing cancer. That’s why I joined myCancerConnection, MD Anderson’s one-on-one cancer support community. I want to be part of a support system for someone else.
When you start out as a new patient, it’s so powerful to meet someone in the waiting room or an online forum who is ‘future you’ -- someone who is in remission or their cancer is stable. When I meet someone going through cancer treatment, I tell them, “I’m future you, and you can do this.”
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
Related Cancerwise Stories

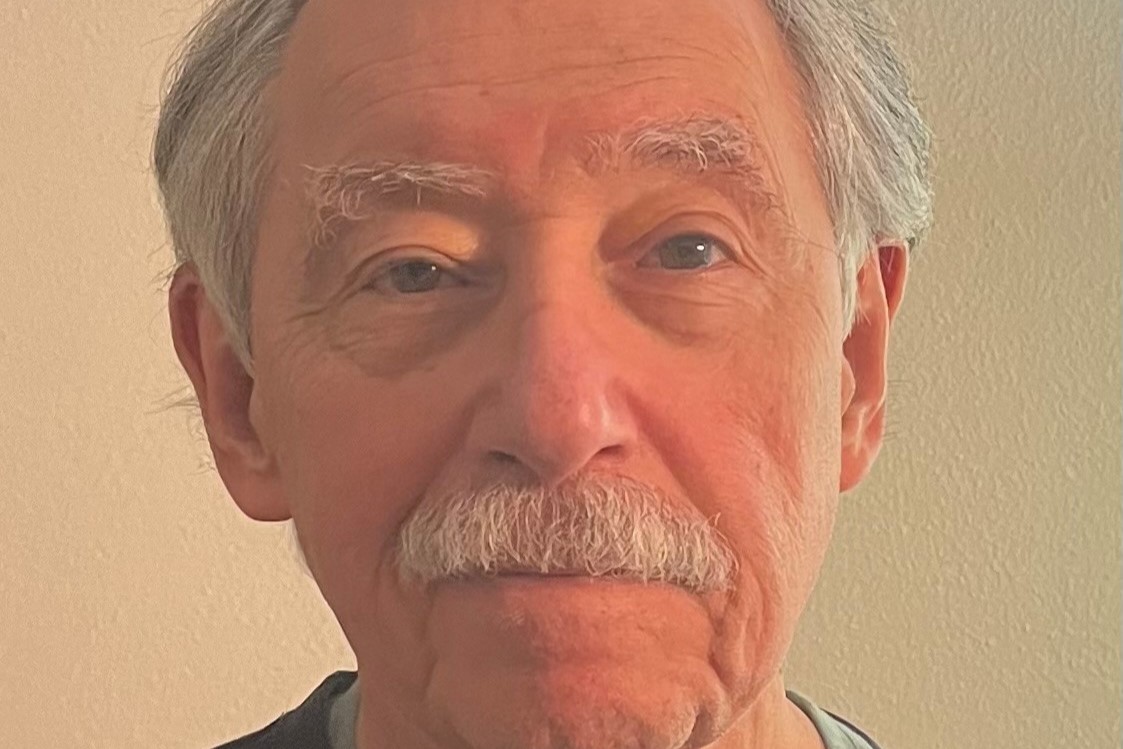
When I meet someone going through cancer treatment, I tell them, ‘I’m future you, and you can do this.’
Elayne Gorhum
Survivor