- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
How diversity within a cancer can influence a patient’s response to treatment
5 minute read | Published October 21, 2020
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on October 21, 2020
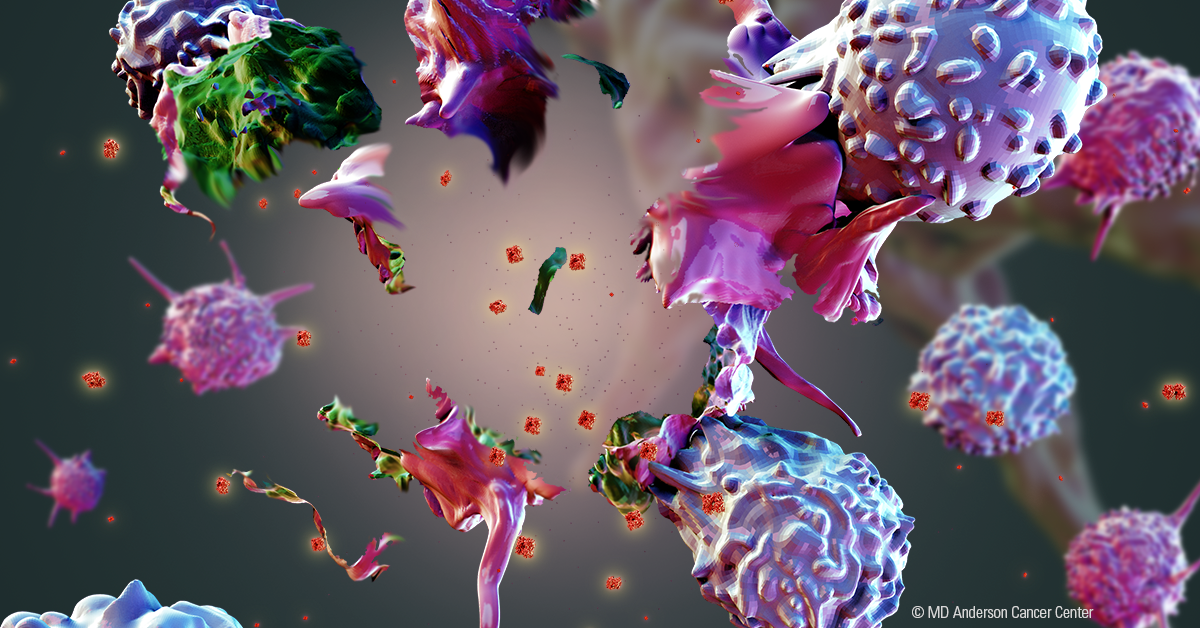
Although a tumor may start from a single cancer cell, it can eventually become millions of cells with unique characteristics. This diversity within cancers has become more apparent with newer analytical tools, and now researchers are beginning to understand how it influences responses to therapy.
A new study from MD Anderson physician and researcher Koichi Takahashi, M.D., Ph.D., describes a technique to study these unique groups of cancer cells. A better understanding of this clonal diversity could have implications for personalizing cancer care in the future. He spoke with us about the study.
What is clonal diversity in cancer?
In the old days, we thought that cancers were made of many identical cells, all with the same features and mutations. The idea was that one bad cancer cell just kept making copies and developed into a tumor.
We have started to learn actually that cancers are quite diverse in terms of their cells. Each cell has a different genetic background. That is clonal diversity; there are distinct groups of cancer cells within a patient.
Why were you interested in studying clonal diversity?
As cancer care has grown more sophisticated, we have developed many targeted therapies that work against specific genetic mutations in cancer cells. We now know that clonal diversity is part of the reason why these treatments may fail or why a patient may experience a relapse.
The treatment might work against most of the cells in a tumor and you may see it shrinking, but there could be a small percentage of cells that are resistant to that treatment. They eventually cause the treatment to fail.
We study clonal diversity then to better understand why treatments fail and how we can overcome that. Diversity is shaped by the evolution, so this research also gives us a snapshot of the evolution of a cancer, which helps us to understand how the cancer started and changed during its growth. You can almost review the tape of the tumor’s development, which can help us to understand what caused it.
How do you study the differences between individual cancer cells in a tumor?
We utilize a relatively new technology called single-cell sequencing. This has revolutionized our research because it allows us to sequence and analyze the DNA of individual cancer cells one at a time.
When we sequenced tumor DNA in the past, we essentially collected DNA from a piece of the tumor and mixed all those cells together and analyzed them as a bulk. This is called bulk sequencing, and that technique gives you a sort of average of the whole tumor. You lose any information about cell-to-cell diversity within the tumor.
An analogy often used to explain this is a smoothie. When making a smoothie, you put all the ingredients in a blender and mix until they’re smooth. When you’re drinking that smoothie, it might not be easy to taste all the separate ingredients – you taste the mixture.
With single-cell sequencing, we can analyze those ingredients before they’re blended and get the genetic information from each cancer cell. In this study, we used the technique to describe the diversity of cancer cells within acute myeloid leukemias, but these methods could be applied to all cancer types.
What were some of your key findings in this research?
We were able to describe the clonal diversity within each patient. Within each patient, there were an average of four distinct cancer cell groups -- what we call subclones. They are related to one another but distinctly different. Some patients had as many as 14 cancer subclones.
This is huge to understand, because it means we’re essentially dealing with 14 different leukemia cell types in that patient. They all have a different configuration of mutations and may respond differently to treatment.
We also studied the evolution of cancer cells within patients to see the history of how the cancer developed. In about half the patients, the changes occurred in a linear fashion. For example, mutation A leads to mutation B and then to mutation C.
In the other half, we saw branching evolution. That would mean mutation A would lead to mutation B as before, but then some cells get mutation C, others would get mutation D, and others would get mutation E. So you end up with mixtures of mutations A-B-C, A-B-D and A-B-E.
What’s really interesting is we saw convergent evolution. That means mutations C, D and E are in different genes or different types of mutations but cause the same functional change within the cancer cell. That suggests that the environment within our bodies leads cancer along similar paths. That’s helpful for us to understand because we might be able to target all of those mutations with a single therapy.
How can your research be used to improve patient care?
For a small number of patients, we were able to perform the analysis in samples collected at diagnosis, when the patient responded to treatment and when a relapse occurred.
We were really able to understand the dynamics of the cancer while the patient was responding to treatment and when the treatment failed. We can see that some subclones disappear during treatment, but small percentages of cells remain behind, grow and eventually cause relapse. We were able to pinpoint in those instances the cause for the relapse.
We’ve only done this for a limited number of patients in this study but applying this routinely in the future could help us to learn quite a bit. Perhaps in the future, we can design better therapy combinations to prevent those subclones from surviving and causing relapse. This all fits within our broader efforts of precision medicine, where we strive to give the most tailored treatment we can to a patient.
More information about the paper, including collaborators, funding support and disclosures can be found here.
Request an appointment at MD Anderson online or by calling 1-855-595-7343.
Related Cancerwise Stories
We study clonal diversity then to better understand why treatments fail and how we can overcome that.
Koichi Takahashi, M.D., Ph.D.
Physician & Researcher