- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Highlighting hope for bladder cancer, cervical cancer and endometrial cancer with fluorescence
3 minute read | Published January 15, 2014
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on January 15, 2014
If you've been in the dark about advances in cancer surgery, look no further than the emerging field of minimally invasive operations aided by fluorescence.
New technologies make it possible to highlight and eradicate more cancer cells in real time using fluorescent dyes and endoscopic instruments with filtered light. Patients hardly can tell the difference from traditional surgery, especially when they're spared future recurrence from otherwise hidden cancer cells.
While fluorescence isn't appropriate for every case, surgeons in Urology and Gynecologic Oncology are especially excited about two new uses.
New hope for bladder cancer patients
H. Barton Grossman, M.D., clinical professor in Urology, helped prove the effectiveness of fluorescence cystoscopy as principal investigator of a large, randomized study of bladder cancer patients in 2007.
Grossman followed more than 800 patients over nine months in conjunction with more than 20 other institutions. Patients were injected with a colorless solution (hexaminolevulinate hydrochloride) through a catheter. Then surgeons looked at the bladder first under traditional white light cystoscopy, then with cystoscopy using blue light. They proved "blue light" cystoscopy better distinguished the parameters of papillary tumors, making them easier to find and remove, presumably reducing tumor recurrence rates.
Another study, published in 2012, continued following the patients. It verified that those who received blue light cystoscopy had improved time to recurrence (16.4 months) compared to those who only had traditional white light cystoscopy (9.4 months).
While this technology has been used in Europe for a number of years, the 2007 study solidified its approval in the United States by the Food and Drug Administration. Today, blue light cystoscopy is nationally marketed as Cysview® and used at a handful of U.S. medical institutions, including MD Anderson, to help detect both papillary tumors and carcinoma in situ (which is characterized by flat malignant lesions on the bladder wall that haven't metastasized).
Grossman has learned to distinguish opportune cases and times for the technology. Using it right after biopsies or where there's inflammation, for instance, may cause false-positive results by highlighting non-cancerous areas of the bladder.
A future of possibilities for cervical and uterine cancer patients
Another minimally invasive technology with far-reaching potential is Firefly™ Fluorescence Imaging for the da Vinci® Surgical System for robotic surgery.
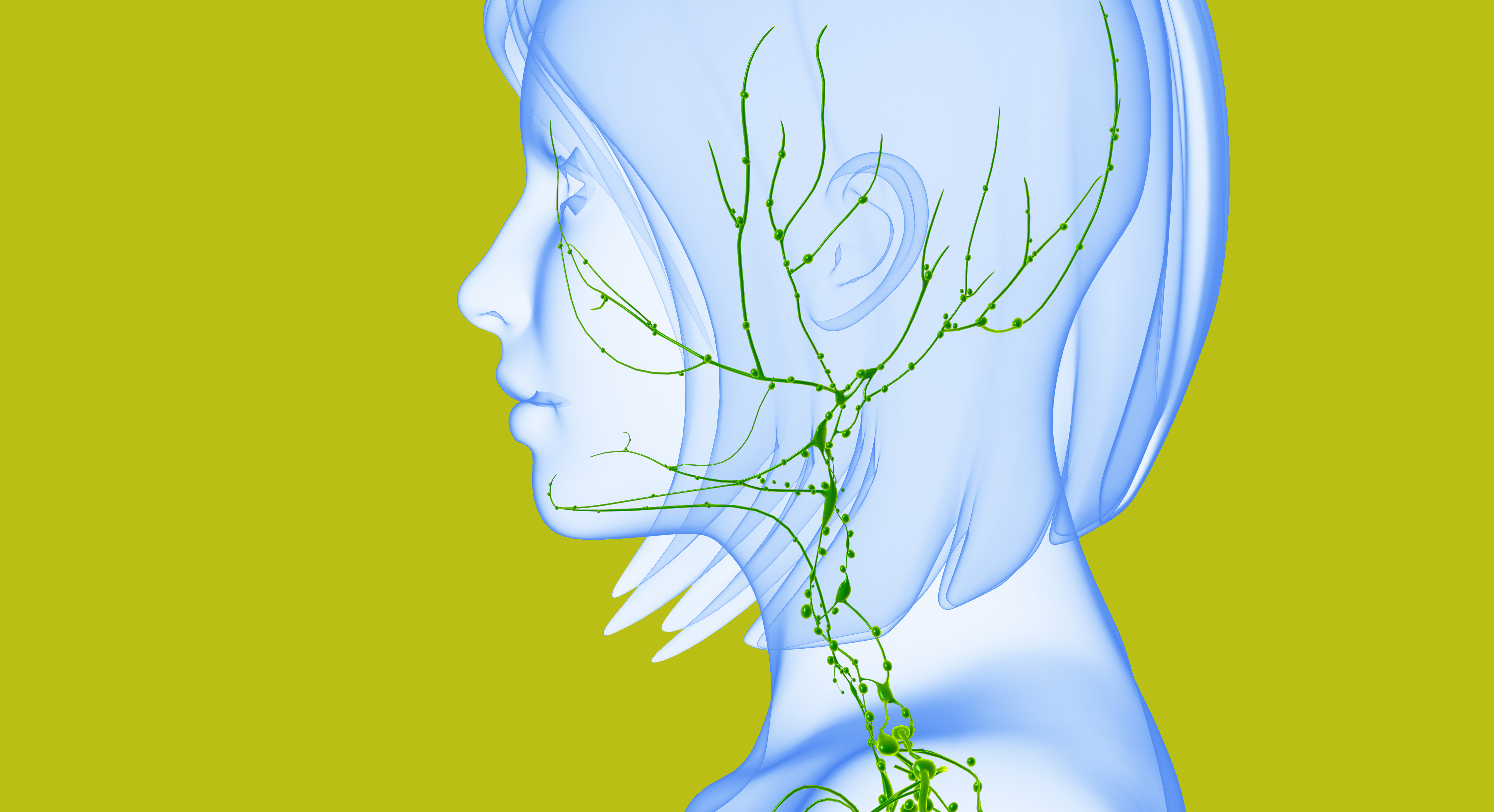
The technology uses indocyanine green (ICG) dye to illuminate blood vessels to identify tumor perfusion and lymphatic channels - and ultimately recognize lymph nodes possibly involved with cancer cells.
Nicole Fleming, M.D., assistant professor in Gynecologic Oncology and Reproductive Medicine, calls it night vision for robotic surgeons.
"It's currently being used both intravenously to look at blood supply to an organ and its adjacent tumor mass and to map lymphatic channels from the tumor to adjacent lymph nodes," she explains. "It illuminates the target, not the entire surgical field, when you activate the fluorescent light."
Fleming's target is typically the sentinel (first) lymph node absorbing cervical or uterine cancer cells. By toggling the da Vinci robotic system between normal and fluorescent lights, she can follow the migration of the ICG dye through the lymphatic system to identify the sentinel node arising from the patient's known cancer. The lymph node identified with ICG dye glows under the fluorescent camera and is submitted for extensive sectioning to determine if microscopic metastases are present.
Better understanding of the lymphatic mapping of these cancers may one day lead to less invasive and smarter lymph node assessments, sparing patients complications, such as lymphedema, after numerous benign lymph nodes have been removed.
"I think this is just the start of where we're going with this," Fleming says.
A longer version of this blog post originally appeared in Messenger, MD Anderson's bimonthly publication for employees.
Cysview® is a registered trademark of Photocure ASA and is used in conjunction with the Karl Storz Photodynamic Diagnostic D-Light C (PDD) System for blue light cystoscopy in the U.S. Firefly™ and da Vinci® SI are trademarks and registered trademarks of Intuitive Surgical, Inc., respectively.
Related Cancerwise Stories

It illuminates the target, not the entire surgical field, when you activate the fluorescent light.
Nicole Fleming, M.D.
Physician