- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
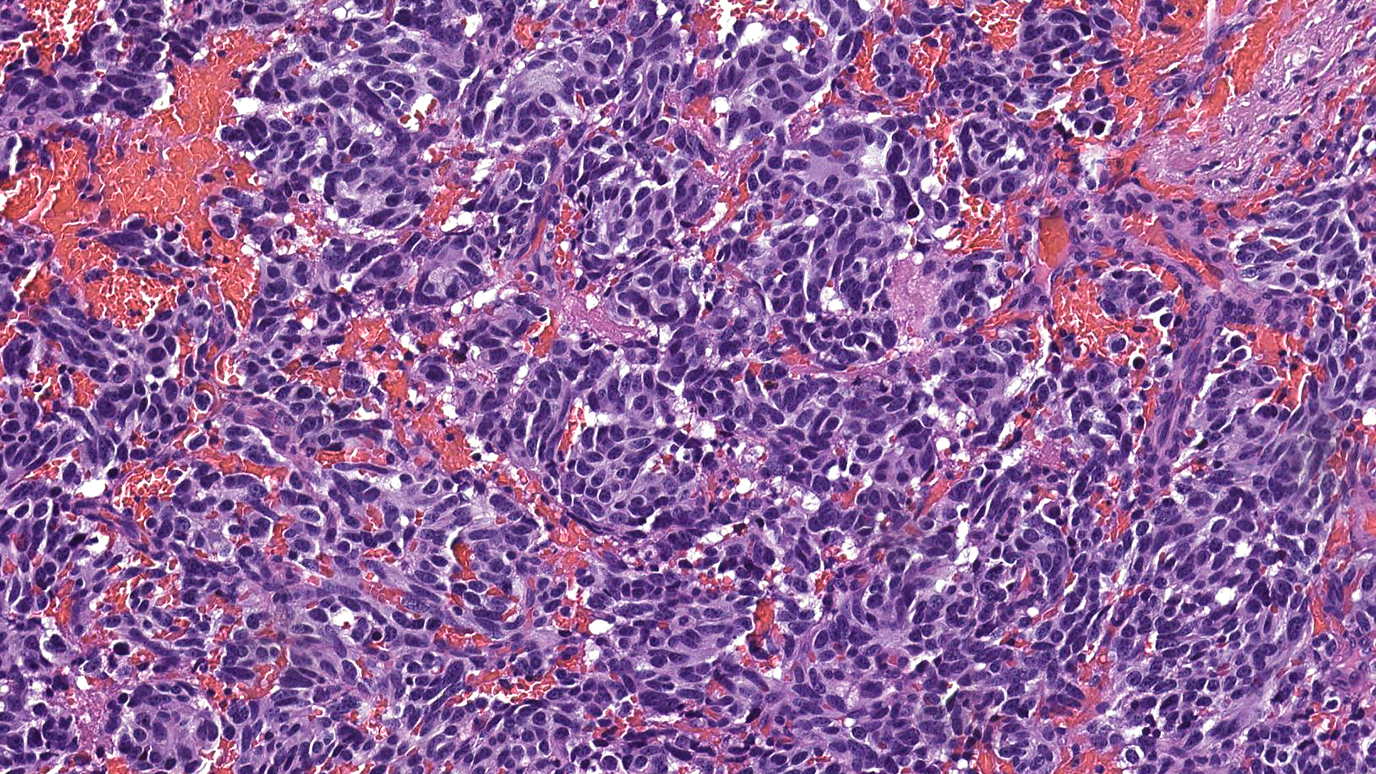
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
Hematochezia vs. melena: What’s the difference?
4 minute read | Published February 07, 2025
Medically Reviewed | Last reviewed by Madhulika Eluri, M.D., on February 07, 2025
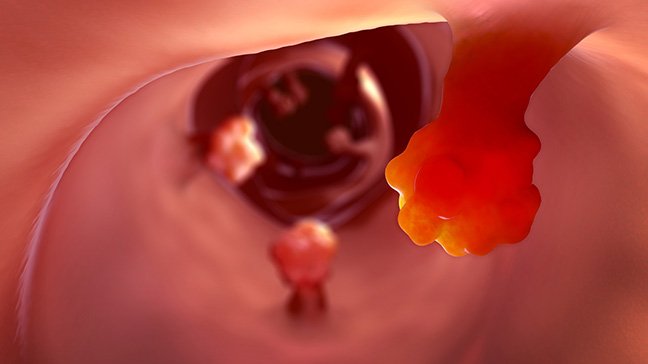
Hematochezia and melena are two terms that describe different ways blood can appear in your stool.
- Hematochezia is bright red blood that generally starts lower in the digestive tract.
- Melena generally starts much higher up in the digestive tract and results in black, tarry stools.
Both melena and hematochezia can be signs of cancer somewhere along your gastrointestinal tract. But can they ever be a symptom of something else?
We went to gastrointestinal medical oncologist Madhulika Eluri, M.D. Here's what she shared.
How are hematochezia and melena pronounced?
Hematochezia is pronounced “hee-mat-oh-KEE-zee-uh.” Melena is pronounced “meh-LAY-nuh.”
What are the main causes of hematochezia and melena?
Aside from cancer, there are many possible causes for both of these symptoms.
The most common cause of hematochezia is diverticulosis, or tiny pouches that develop in the colon wall and get clogged with fecal matter and/or infected. Other possible causes of hematochezia include:
- Hemorrhoids: internal or external
- Inflammation of the colon: possibly due to inflammatory bowel disease (IBD)
- Infection: due to ulcerative colitis or some other condition
- Vascular lesions: also known as angiodysplasia
The most common causes of melena are stomach ulcers and inflammation of the esophagus or stomach. But other possible causes include:
- Varices: This complication of portal hypertension leads to engorged blood vessels in the GI tract. If the pressure gets high enough, the vessels can start bleeding.
- Vascular lesions: These are problems with the blood vessels themselves, which could be hereditary or due to chronic kidney or heart disease. They can be aggravated by certain medications, such as NSAIDs.
- Trauma: Possibly due to a Mallory-Weiss tear, this is a small rip in the lining of the digestive tract at the juncture of the stomach and esophagus. It is usually associated with prolonged vomiting or retching.
But blood in your stool can also be a sign of cancer. That’s why it’s so important to be examined by a gastroenterologist.
There’s no way to tell what’s causing blood in your stool without a thorough evaluation. This will likely include a comprehensive medical history and may include upper and lower endoscopies. Procedures like these allow us to inspect the entire length of the gastrointestinal tract and see the source of blood with our own eyes.
Is hematochezia or melena considered urgent? How quickly should I see a doctor?
It’s normal to be scared any time you see blood in your stool. But these symptoms can also be caused by several benign — or non-cancerous — conditions.
Whether your situation is urgent depends on the amount of blood you’re seeing and other factors. You should go to an urgent care clinic or emergency room right away if you have any of the following symptoms in addition to blood in your stool:
- Dizziness
- Severe or worsening abdominal pain
- Vomiting blood
- Weight loss
Key points
- You need to see a doctor any time you see blood in your stool.
- Hematochezia and melena can be caused by both benign and cancerous conditions.
- There’s no way to tell what’s causing blood in your stool without an examination.
What do hematochezia and melena actually look like?
Hematochezia is usually bright red because it starts much lower in the digestive tract. Patients with diverticulitis sometimes report there’s so much of it that it looks like the toilet bowl is filled with blood. That can be really scary.
Melena usually appears as black, tarry stools. This is because hemoglobin (a blood protein) gets much darker as it passes through the gastrointestinal tract and is exposed to digestive enzymes that break it down.
Iron pills can sometimes make stools appear dark, but that’s not because they cause any bleeding. Patients often can’t tell the difference, though. That’s why it’s so important to be evaluated. We might need to review your medications and do some lab work, too.
Do hematochezia and melena ever go away on their own?
If you have a bleeding stomach ulcer, it’s possible that it could stop and restart. That may also be true of inflammatory bowel disease. But when you’re talking about a tumor or cancer, bleeding doesn’t usually go away on its own.
Is there anything I should avoid eating while experiencing hematochezia or melena?
You should stop taking NSAIDs like ibuprofen or acetaminophen since these can cause stomach irritation and bleeding. Similarly, if you’re taking any type of blood thinner, discuss that with your doctor. But in terms of diet, you don’t need to change anything. There’s no particular food that you should avoid.
How are hematochezia and melena usually treated?
That depends on what’s causing them, since both can be due to cancer and non-cancerous conditions. That’s why an evaluation by a gastroenterologist is crucial.
What’s the single most important thing to know about hematochezia and melena?
You need to see a doctor any time you see blood in your stool. Colorectal cancer is being diagnosed in a growing number of young people. We’re seeing more rectal cancer cases in particular in people under age 50. Historically, these patients have been told that they just have hemorrhoids. So now, it’s even more important to have a full evaluation performed by a gastroenterologist to make sure you get an accurate diagnosis.
Blood in your stool can be caused by many things, and most of those are unrelated to cancer. But it’s still important to get checked out if you see it.
Request an appointment at MD Anderson online or call 1-877-632-6789.

These symptoms can also be caused by several benign conditions.
Madhulika Eluri, M.D.
Physician