- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (718)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (164)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (124)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (898)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1776)
Deep vein thrombosis as a side effect of cancer: 9 things to know
5 minute read | Published September 14, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on September 14, 2023
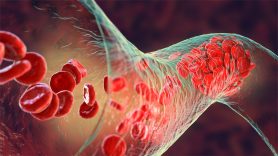
The risk of developing blood clots is somewhat higher among cancer patients. This is due both to the inflammatory nature of the disease itself and the therapies used to treat cancer.
Deep vein thrombosis (DVT) is one such type of blood clot. It forms in the veins found deep inside muscles and other tissues, and it can be fatal if left untreated.
Why are cancer patients more susceptible to DVT? And, can it be prevented? We asked breast medical oncologist Ajit Bisen, M.D., for insight.
Why are cancer patients at increased risk for deep vein thrombosis?
Our bodies have a natural ability to balance blood clotting with blood flow. But whenever you introduce a variable into the mix, it causes an imbalance that can lead to the development of blood clots, including DVT.
Cancer is considered a “hypercoagulable” condition because it’s more likely to lead to blood clots. That’s because both cancer and its treatment often create one or more of the conditions necessary for blood clot formation. Collectively, they’re known as the Virchow triad:
- a change in blood flow,
- a blood vessel injury, or
- a change in the composition of the blood.
Cancer causes inflammation, which can make blood more likely to clot. Tumors can cause blockages and issues with blood flow. And surgeries and radiation therapy can cause injuries to tissue, sometimes even at the microscopic level. So, any or all of these could contribute to DVT.
Where do cancer patients typically develop deep vein thrombosis?
The most common place is one of the legs, simply because gravity tends to make blood pool at the bottom of the body. But it can also develop in the arms, neck, chest or abdomen.
In cancer patients, DVT sometimes forms at the site of a chemotherapy port, too. It’s a type of catheter inserted into one of the deeper veins of the chest. It can cause injury to the vein and can affect blood flow, leading to DVT.
And, if the body identifies the port as a foreign object, it can activate the “coagulation cascade,” an assembly of proteins and clotting factors that normally converge on the site of an injury to stop the bleeding. This balance between bleeding and clotting happens at the site of any tissue injury.
Does deep vein thrombosis have any symptoms?
The most common symptoms of DVT among cancer patients are:
- arm or leg: swelling, redness and pain in the area of the clot
- abdomen: abdominal pain
- chemo ports: swelling or redness around the port
How is deep vein thrombosis usually found in cancer patients?
Sometimes, patients will come to the clinic reporting one or more of the symptoms described above. But often, it’s just an incidental finding on CT scans that are performed to stage cancer.
What are the biggest risk factors for deep vein thrombosis?
We divide DVT into two categories: “provoked” and “unprovoked.”
Provoking risk factors include:
- not getting up to move around very much during extensive travel
- major surgery causing vascular injury, prolonged hospitalization and/or limited mobility
- trauma fractures, such as a broken leg or rib
- malignancies requiring active treatment
- medications, such as estrogen therapy
- high body weight
- pregnancy
- smoking
- inherited conditions such as factor V Leiden, antiphospholipid syndrome and autoimmune disorders.
All of these may contribute in some way to an imbalance.
Unprovoked DVT has no clear explanation for its cause.
How is deep vein thrombosis treated?
If DVT is due to a clear, provoking reason that’s considered a transient risk factor, we’ll normally treat it for about 3 to 6 months with blood thinners. We have several different types to choose from. These help stabilize the blood clots and keep them from getting any bigger.
Quick-acting clot-busting medications called thrombolytics are not usually used unless you’re in a life-threatening situation, such as a stroke, heart attack, or a large pulmonary embolism. That’s when a blood clot dislodges from its original location and travels to the lungs, where it can block an artery. That condition is very dangerous and can sometimes be fatal.
If you have a persistent risk factor such as cancer, an autoimmune disorder, or chronic organ dysfunction, we’ll treat you for as long as the risk factor is present. In stage IV cancer patients, that could mean for the rest of your life.
When should you seek help for possible DVT?
Deep vein thrombosis can turn fatal very quickly by dislodging and traveling to the lungs, so notify your provider immediately about any new swelling associated with pain or redness. They may start you on a blood thinner right away.
But if you’re also experiencing shortness of breath, chest pain, lightheadedness or difficulty breathing, call 911.
What’s the one thing you want cancer patients and their caregivers to know about DVT?
Blood clots are a very common side effect of cancer. And aside from the cancer itself, they are the second most common cause of death among cancer patients. So, if you think you might be developing one, don’t wait. Contact your care provider right away and get it checked out.
Can deep vein thrombosis be prevented?
There are a few things you can do to reduce your risk of blood clots.
Sometimes, even otherwise healthy people will notice some ankle swelling if they’ve been sitting in the same position for a long time, like on a transatlantic flight. So, try to avoid long periods of inactivity or immobility. Get up and walk around frequently to keep your blood flowing, whether you’re in your car on a long trip or sitting at your desk or on the sofa.
If you have any injury to your legs or body, be vigilant about watching yourself for symptoms.
If you’re carrying excess body weight, look into weight loss programs.
And if you smoke, quit now. Medication and counseling are the best ways to do it. Call 1-800-784-8669 or text QUIT to 47848. Cancer patients can also enroll in MD Anderson’s Tobacco Research and Treatment Program.
Request an appointment at MD Anderson online or by calling 1-877-699-1113.
There are a few things you can do to reduce your risk.
Ajit Bisen, M.D.
Physician