- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
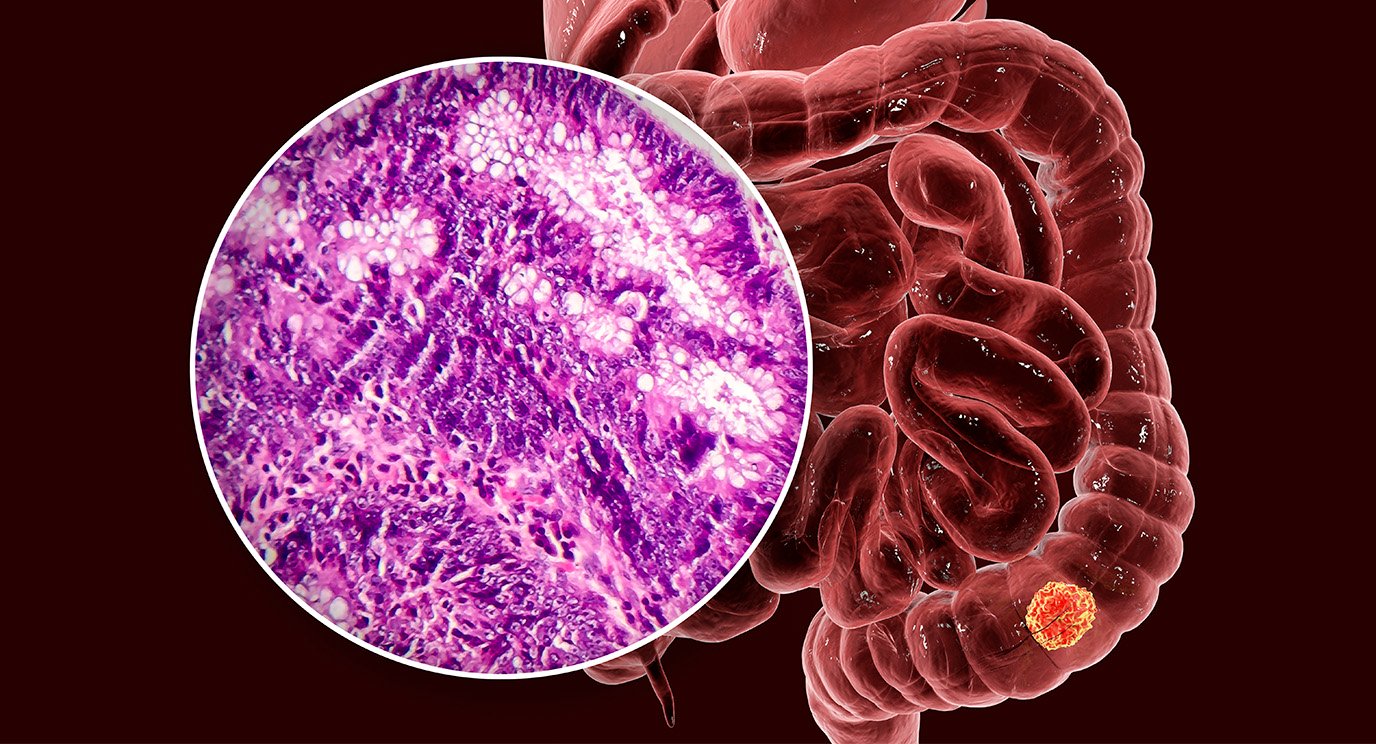
Colon polyps: 10 things to know
4 minute read | Published March 03, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on March 03, 2022
If you’re age 45 or older, your doctor may have already talked to you about the need to start getting a colonoscopy to check for polyps.
But what are colon polyps? Who gets them? And why do they need to be removed? We checked in with gastroenterologist David Richards, M.D.
What is a colon polyp?
I usually describe it as a little growth that develops in the lining of the large intestine, or colon.
Who typically gets colon polyps?
Men are more likely to develop colon polyps than women. But getting older is also a risk factor for developing polyps, which is why it’s recommended that people start having colorectal cancer screenings at age 45. Colonoscopy is the preferred method of screening for colorectal cancer.
Certain genetic syndromes can also predispose people to developing colon polyps and colorectal cancer. So, patients with Lynch syndrome or familial adenomatous polyposis will require earlier and more frequent follow-up. A significant family history of colon polyps, particularly pre-cancerous polyps, may also result in more frequent monitoring, and potentially earlier monitoring, than average-risk patients.
What do colon polyps look like?
Colon polyps can appear in a number of ways:
- Pedunculated: A little ball of tissue on the end of a stalk, like a broccoli floret or a mushroom.
- Sessile: A smooth bump or a gradually sloping “hill” on the lining of the colon.
- Flat: These are often very hard to see, as they may have no visibly raised portion at all.
- Depressed: In rare cases, patients may have a small dip or depression in the lining of the colon.
Is a colon polyp the same thing as a hemorrhoid?
No. Though they can bulge out of the colon wall when inflamed, too, hemorrhoids are just veins in the anal or rectal area that get swollen or irritated.
Are all colon polyps pre-cancerous?
No. Some abnormal growths can actually be benign. And there are several different kinds of colon polyps. Not all of them will turn into cancer. Even those that could turn into cancer someday aren’t necessarily guaranteed to. They just have the potential. That’s why they’re considered “pre-cancerous,” and looking for them during a colonoscopy is a standard part of colorectal cancer screening.
Which types of colon polyps are considered the most concerning?
Certain colon polyp features are more worrisome than others, but shape is not generally among them. The three things we tend to focus on most are:
- Size: Anything bigger than about 1 cm, or the width of a AAA battery
- Number: The more pre-cancerous polyps someone has, the higher their risk will be. So, someone with 1 or 2 small polyps is at less risk than someone with 3-9. And so on.
- Histology: This just means the way a polyp’s cells appear under a microscope. We examine their shape, as well as the order and way in which they grow, to look for abnormalities.
Do colon polyps cause any symptoms?
The vast majority of people with polyps have no symptoms at all. But polyps can sometimes cause bleeding, which ranges from microscopic levels that only show up as iron-deficiency anemia, to black tarry stools, to bright red blood. In rare cases, they might also cause some minor rectal discomfort or large amounts of mucus to be passed.
How are colon polyps removed?
Most colon polyps can be removed during a colonoscopy. That’s one reason doctors like colonoscopies so much. We can actually see the growths with our own eyes and remove them on the spot. And we’ve gotten so good at removing polyps with scopes now that very, very few patients need surgery to accomplish that.
Most polyps are removed with simple devices such as forceps or snares, which are introduced through the scope itself. If those methods aren’t feasible, polyps can be removed using a procedure called endoscopic mucosal resection.
Polyps can also be removed with a highly specialized procedure called endoscopic submucosal dissection. One of my colleagues, Dr. Phillip Ge, performs that technique quite a bit. It requires significant expertise, and is good for removing large polyps and early-stage colorectal cancers, too.
Which procedure is called for depends entirely on each patient and their unique situation. But the really cool thing about endoscopic submucosal dissection is that doctors are actually able to burrow underneath a polyp, getting between the colon lining and the muscles, and cut it out from below. That way, doctors can take out really big polyps in one chunk, rather than multiple fragments. And that’s important, because any time something is being taken out in pieces, rather than as a whole, there’s a small chance that a cell or two might be left behind where it could grow back.
How will the discovery of colon polyps impact my follow-up screening schedule?
If you have a lot of polyps, or they’re very large or pre-cancerous, you might need to be scoped more often. But it really depends on what kind of polyps are found and what their cells look like under a microscope.
If you had a really big polyp removed using endoscopic mucosal resection, you would also need to be followed much more closely. So, your doctor might recommend being scoped more frequently.
What’s the one thing you want people to remember about colon polyps?
Polyps themselves are not cancer. Some just have the potential to develop into it. We remove them so they never have that chance.
Request an appointment at MD Anderson online or by calling 1-877-966-0244.

Some abnormal growths can actually be benign.
David Richards, M.D.
Physician