- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Cervical cancer symptoms: What to look for and when to see a doctor
3 minute read | Published November 11, 2022
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on November 11, 2022
Like many women diagnosed with cervical cancer, Linda Ryan didn’t initially have any symptoms. So, she didn’t know she had the disease until a routine Pap test came back abnormal after a well-woman exam in 2004.
Unlike many women, though, Linda has also had six separate recurrences. And, no two back-to-back cervical cancer recurrences were caught in precisely the same way.
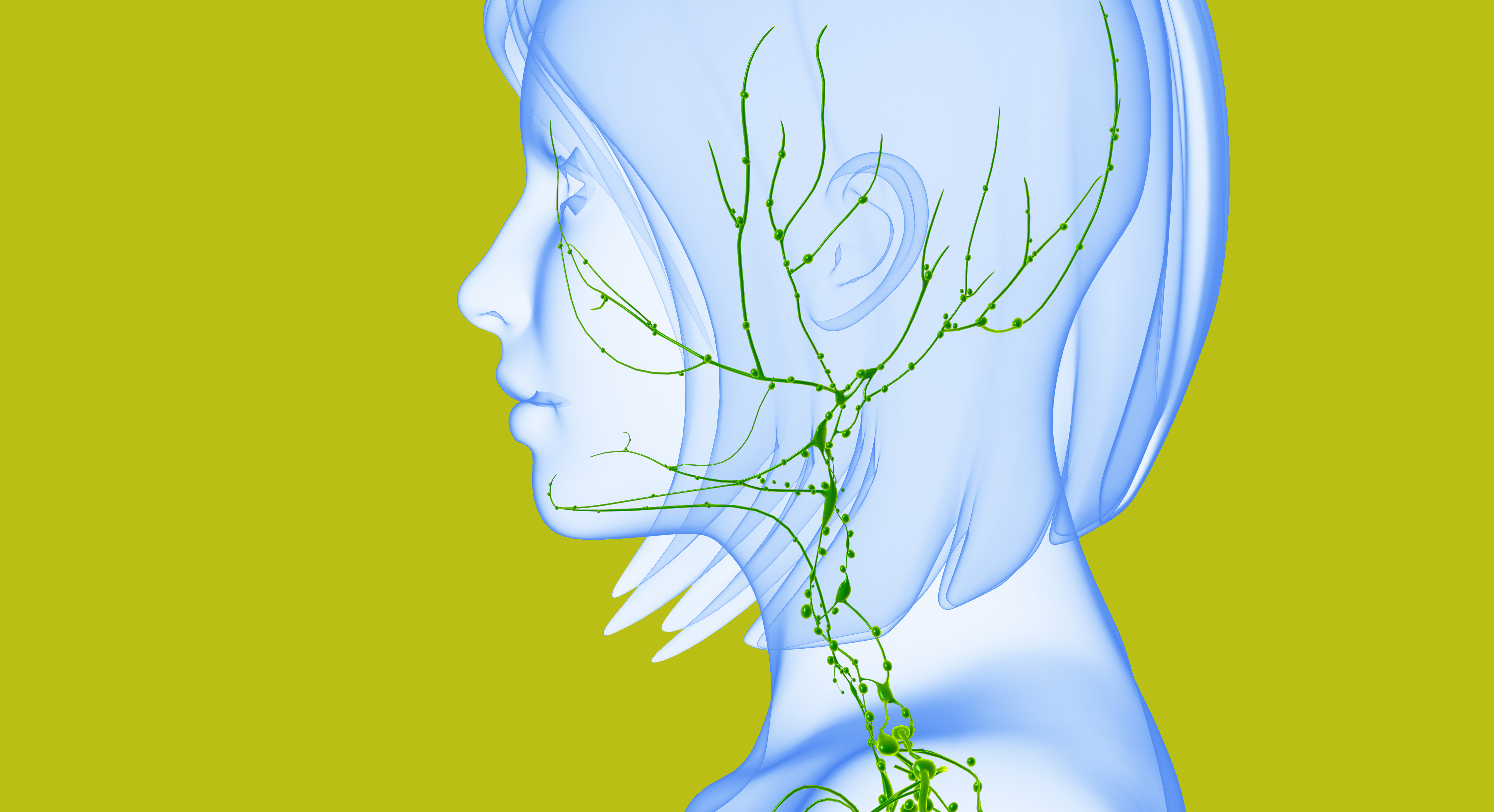
With the first and third, Linda noticed swollen lymph nodes in her neck and/or groin. Another caused pelvic discomfort. Two more showed up on regular scans. And the latest caused alternating constipation and diarrhea because cancer had formed a tumor in her rectum.
“Having trouble going to the bathroom is such an unpleasant thing to talk about,” Linda notes. “But that was the truth of my experience. I’ve never had the bleeding that some people describe.”
Abnormal bleeding and other symptoms of cervical cancer
Cervical cancer in its earliest stages may not have any symptoms. But when women do have symptoms, abnormal vaginal bleeding is among the most common.
That could mean anything from a faint tinge of pink in otherwise clear vaginal discharge to extremely heavy menstrual periods. It could also mean bleeding after sex, bleeding between periods, or even spontaneous vaginal bleeding after menopause.
“I started having this watery discharge between my periods, and then really, really heavy menstrual cycles,” remembers Shalee Landry, who was 37 when she was diagnosed with cervical cancer in 2012. “I’d never had heavy periods like that before. I thought it was caused by stress.”
Other, less common symptoms of cervical cancer include:
- pelvic pain
- feeling bloated or full
- pain that radiates to the legs or back.
“It’s not unusual to experience irregularities in your cycle just before menopause,” notes Jolyn Sharpe Taylor, M.D., a surgeon specializing in gynecologic cancers. “And it’s important to talk to your doctor about those issues. But if you experience heavier than usual bleeding, bleeding in between your periods, bleeding after sex or bleeding after menopause, don't wait to contact your doctor.”
HPV increases the chances of a cervical cancer diagnosis
When watching for cervical cancer signs, your HPV status is another factor. The human papillomavirus (HPV) causes several types of cancer in both men and women — including cervical cancer.
A second positive HPV test is how Sylvia Zaro found out she had cervical cancer in 2016, at age 46.
“I’d been having Pap tests and HPV tests done regularly for more than 20 years,” she explains. “I never had an abnormal result until 2015. So, I was surprised.”
Fortunately, none of the strains that can cause cancer were detected in Sylvia’s 2015 tissue sample. So, her doctor recommended waiting a year and then getting retested.
In 2016, Sylvia tested positive for HPV again. But this time, it showed evidence of the strains that could cause cancer. Sylvia’s doctor performed a colposcopy to see if she’d already developed it. “To my surprise, those results came back positive, too,” Sylvia says.
That’s why it’s so important to stay current on your follow-ups if you have a positive HPV test or abnormal Pap test of any kind.
Get vaccinated against HPV, if eligible
Everyone ages 9-26 should get the HPV vaccine. In addition to preventing most cervical cancers, the vaccine prevents most anal, penile, vaginal and vulvar cancers, plus HPV-related throat cancers.
If you are ages 27-45 and are unvaccinated, talk with your doctor about the possible benefits of getting the HPV vaccine. The vaccine is proven to be safe and effective at preventing infection from nine strains of HPV that are linked to cancer and genital warts.
“The majority of cervical cancer cases are associated with HPV,” says Taylor. “So, prevention is the best way of avoiding HPV-related cervical cancer and its pre-cancerous relative, cervical dysplasia. Vaccinating boys and girls ages 11-12 is ideal, though as early as age 9 is reasonable, and even receiving the vaccine later can still protect young men and women from strains they might not have been exposed to yet.”
Request an appointment at MD Anderson online or by calling 1-888-501-2254.
Related Cancerwise Stories

It’s not unusual to experience irregularities in your cycle just before menopause.
Jolyn Sharpe Taylor, M.D.
Physician