- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (66)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (28)
- Bladder Cancer (68)
- Brain Metastases (28)
- Brain Tumor (230)
- Breast Cancer (716)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (154)
- Colon Cancer (164)
- Colorectal Cancer (110)
- Endocrine Tumor (4)
- Esophageal Cancer (42)
- Eye Cancer (36)
- Fallopian Tube Cancer (6)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (6)
- Kidney Cancer (124)
- Leukemia (344)
- Liver Cancer (50)
- Lung Cancer (288)
- Lymphoma (284)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (98)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (170)
- Pancreatic Cancer (166)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (144)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (236)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (60)
- Testicular Cancer (28)
- Throat Cancer (90)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (78)
- Vaginal Cancer (14)
- Vulvar Cancer (18)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (624)
- Complementary Integrative Medicine (24)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (230)
- Epigenetics (6)
- Fertility (64)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (122)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (118)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (894)
- Research (390)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (404)
- Survivorship (322)
- Symptoms (184)
- Treatment (1774)
Can leukemia be treated with a pill?
5 minute read | Published December 11, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on December 11, 2023
Leukemia treatments have been constantly improving from the days when patients had to come to the hospital or clinic for intravenous doses of chemotherapy that caused unwanted side effects. Now, leukemia treatment often can be as convenient as a medication taken at home — a pill (or pills) with drugs highly customized to the person’s type of leukemia and even the genetic mutations present within those individual’s cancer cells.
In research presented at the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition, MD Anderson experts shared how different types of leukemia medication can be highly effective as oral treatments.
“It makes it much easier,” says leukemia specialist Nitin Jain, M.D. “Rather than telling the patient to come every day for five days for an IV chemotherapy treatment, we can just prescribe a pill they can take at home.”
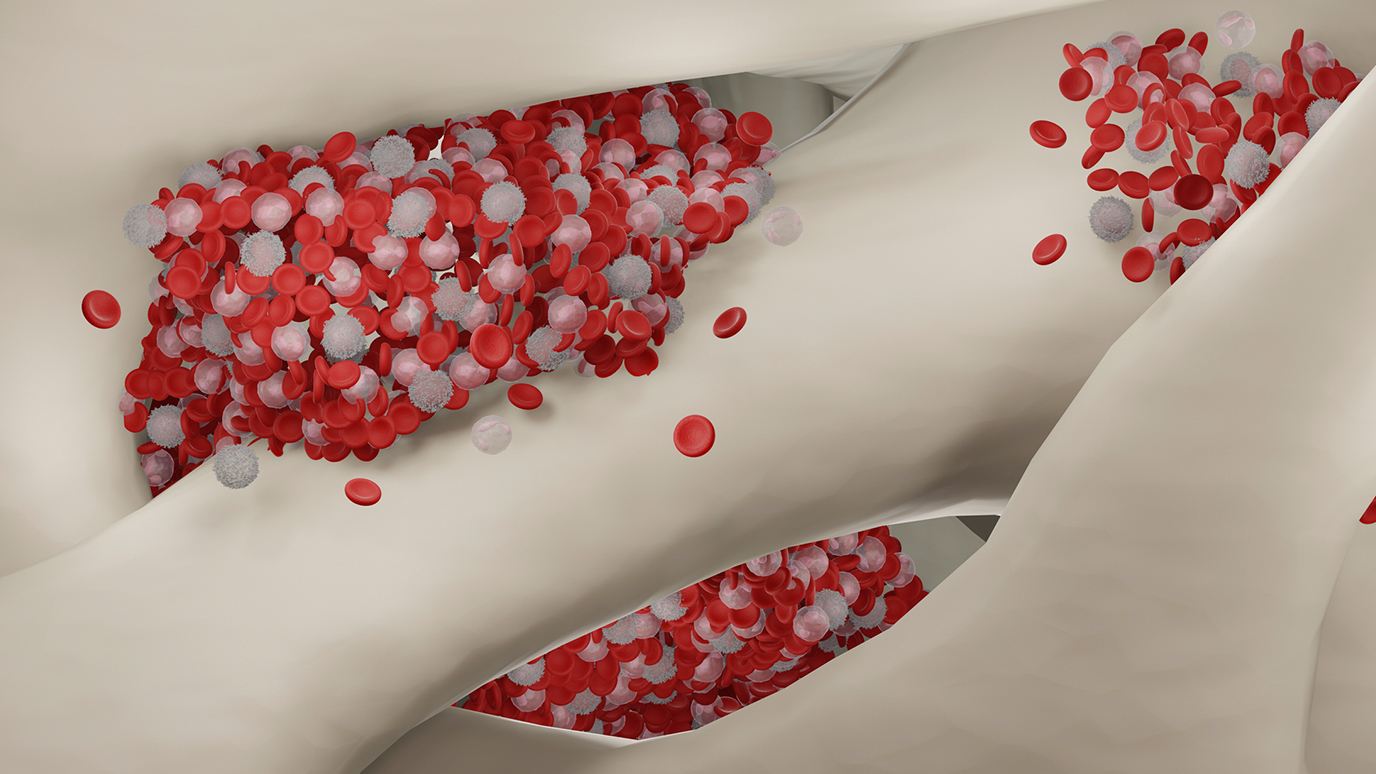
Drug combination showed early success for CLL treatment
In 2019, Jain and his colleagues published the results of an MD Anderson clinical trial in the New England Journal of Medicine in which patients with chronic lymphocytic leukemia (CLL) were given an oral treatment regimen combining two drugs: ibrutinib and venetoclax. This combination included two separate approaches with medications that work through two different mechanisms of action: a BTK inhibitor and a B-cell lymphoma-2 (Bcl-2) protein inhibitor, respectively. One works more in the lymph nodes and the blood, and the other more in the bone marrow. “We get the best out of this drug combination because they have complementary activity and synergy,” Jain says.
The patients — all of whom were older, high risk or both — took the drugs together for two years. “We had high rates of deep remission for our patients,” Jain says. Most stopped taking both drugs after two years, although a few continued taking the combination therapy for a third year.
The researchers recently presented the results of a five-year follow-up at ASH (Abstract 4635). “Many are still in remission after five years,” Jain says. “That is quite remarkable.”
Additional BTK inhibitors are in the pipeline for CLL and potentially other diseases, too
As effective as these drugs are, there is always room for improvement. “There’s this concept of a third-generation BTK inhibitor, which works in a different mechanism, non-covalently,” Jain says. An example is a new drug called AS-1763.
At ASH, senior research scientist Shady Tantawy, M.D., is presenting a poster (Abstract 1453), coauthored with Jain, indicating the results of their investigation of AS-1763. It showed a highly selective profile for BTK and potent inhibitory activities for several forms of BTK. Based on this encouraging early data, the team is recruiting for a new clinical trial to test AS-1763 for patients for whom other treatments haven’t worked. They hope that this will prove to be another oral drug possibility for patients when other treatments have failed.
New treatments for AML with high response rates
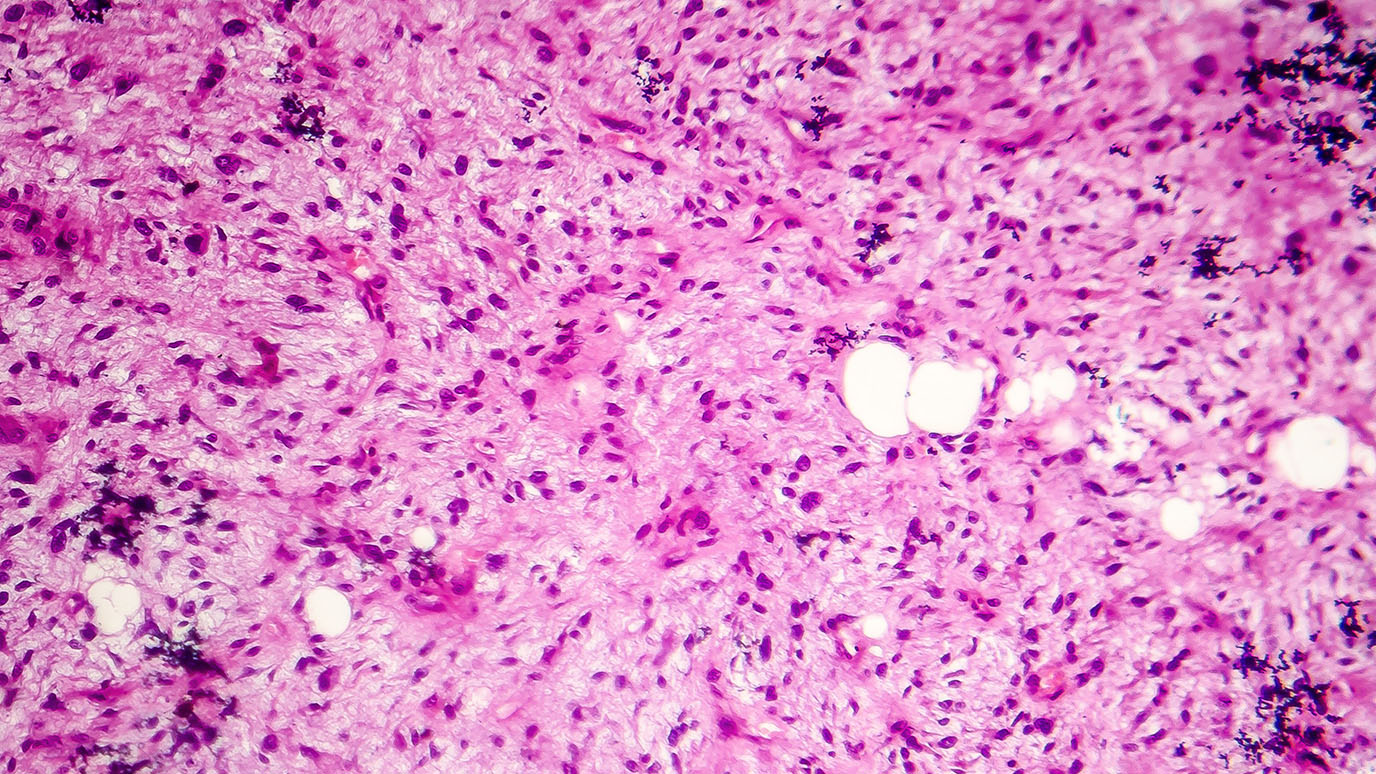
Acute myeloid leukemia (AML) can be thought of as a group of cancers, each with its own mutations. Therefore, the most effective treatments are personalized and targeted, based on both the type of AML and the patient’s age and health status.
Previous research showed that an IV regimen of a hypomethylating agent combined with venetoclax was highly effective in older adults who weren’t good candidates for a more intensive chemotherapy treatment. “This was the first real breakthrough for AML in older patients in decades,” says leukemia specialist Tapan Kadia, M.D. However, the patients have to come into the hospital or clinic every day for a week out of every month for treatment for the rest of their lives.
“We asked ourselves, ‘How can we make this better?’” Kadia says. He and his team in the leukemia department conducted a clinical trial on the use of the drug ASTX727 (which is the hypomethylating agent decitabine/cedazuridine plus venetoclax) in pill form. The results, which Kadia is presenting at ASH (Abstract 833), showed a response rate of 64% among patients in the trial who were newly diagnosed with AML, also known as the frontline patients. Among those with relapsed or refractory AML, the response rate was also high: 46%. The pill was about as effective as the IV form of treatment and had tolerable side effects.
“A 64% response rate, especially in a group of patients with a median age of 80 years, is excellent,” Kadia says. “Overall, in this older and very high-risk population of patients, the regimen was effective and tolerable. Eventually, I hope having the oral option will make the treatment more accessible for people, as they won’t have to come into the hospital or clinic as often.”
Although this study was open to all patients with AML over the age of 75 (in the frontline group) and with AML who hadn’t responded to treatment or that had returned (in the relapsed/refractory AML group), research indicates that targeting the drug based on the specific mutations of the cancer can be even more effective.
Researchers explore treatments for IDH-mutated AML
MD Anderson researchers are also conducting a clinical trial of ASTX727 combined with venetoclax and a targeted therapy in patients with IDH-mutated AML (Abstract 968). These patients have a mutation in either isocitrate dehydrogenase (IDH) 1 or 2, which can be targeted with the inhibitors ivosidenib or enasidenib, respectively. Both drugs can be taken orally.
This study enrolled only patients with mutations in IDH 1 or IDH 2 and treated them with the all-oral triplet of decitabine/cedazuridine (ASTX727) combined with venetoclax and targeted mutant IDH inhibitors ivosidenib or enasidenib. Although the study is still ongoing, the results, presented at ASH by fellow Himachandana Atluri, M.D., so far show 96% of patients with newly diagnosed IDH mutated AML achieved composite remission. In addition, about 45% of patients with relapsed or refractory disease also achieved composite remission. In all groups, some of the patients did have side effects, but these were either mild or could be managed with other drugs, such as corticosteroids.
“The response rates were significantly higher, and the median overall survival was not reached, but is a plateau, and still ongoing,” Kadia says. “In general, it is showing that this all-oral drug triplet regimen is effective and can also be used when other drugs have not worked.”
Looking to the future of leukemia treatment
“The current standards are not necessarily optimal,” Jain says. That’s why he and others are conducting clinical trials to improve upon the efficacy of already-established treatment regimens for different types of leukemia and are enrolling even newly diagnosed patients.
“AML treatment has changed,” Kadia says. “People used to apply a one-sized-fits-all treatment, but for decades now at MD Anderson, we take an individualized approach based on what the patient’s bone marrow shows on molecular testing and genetic tests, such as the IDH mutations. Characterizing the leukemia before starting treatment is paramount.”
“We have made tremendous progress,” Jain says. “Many patients with certain types of leukemia, especially CLL, have an almost-normal lifespan.”
Request an appointment at MD Anderson online or call 1-888-240-0380.

Many are still in remission after five years. That is quite remarkable.
Nitin Jain, M.D.
Physician