Glioblastoma immunotherapy study offers hope
- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (914)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Can immunotherapy treat glioblastoma? Understanding the latest study
BY Meagan Raeke
4 minute read | Published February 25, 2019
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on February 25, 2019
A new study has revived hope for the role of immunotherapy in treating glioblastoma, the most aggressive and deadly form of brain cancer in adults. The study used a type of immunotherapy known as checkpoint inhibitors, which train the immune system’s T cells to fight cancer. Although checkpoint inhibitors have greatly increased overall survival for some types of cancer, such as melanoma, early clinical trials failed – until now – to show any benefit for glioblastoma.
We sat down with John de Groot, M.D., professor and interim chair of Neuro-Oncology, who led the MD Anderson portion of the study, to learn more about the latest progress in immunotherapy for glioblastoma.
How did this clinical trial work?
The Phase II randomized clinical trial was led by researchers from UCLA and conducted at six other institutions, including here at MD Anderson. We enrolled recurrent glioblastoma patients – people whose tumors had returned after their initial treatment. Nearly all glioblastomas recur, and when this happens, median survival drops to less than a year.
The study had two different arms. In one arm, patients received pembrolizumab, an immune checkpoint inhibitor, both before and after surgery. In the other arm, patients only received the drug after surgery.
How was this study different from previous clinical trials studying immunotherapy in glioblastoma patients?
Most glioblastoma clinical trials only give the new drug at the time of recurrence, usually without surgery. Previous studies of pembrolizumab in glioblastoma that were designed this way haven’t shown a survival benefit.
One of the goals of this study was to look at the drug’s effect on tumor biology. In order to do that, we had to design a “window of opportunity” clinical trial, where the drug is first given several weeks before surgery and continued afterwards. Researchers studied the tumor tissue removed during surgery to see how the drug affected the immune cells within the tumor.
Because this trial included two arms, researchers were also able to compare the impact of the drug on the tumor tissue and patient survival between the two treatment approaches.
What did the clinical trial find?
Surprisingly, the study found that glioblastoma patients who received pembrolizumab before surgery survived much longer than those only receiving it after surgery. We didn’t expect for one group to live longer than the other.
The study also found more activated immune cells, including T cells, in the tumor tissue from those who received the drug before surgery.
What does this mean for glioblastoma patients and caregivers?
There is hope that there might be a way moving forward to use immunotherapies more strategically for the treatment of glioblastoma.
One of the most important things to remember about this scientific data is that it needs to be repeated to know if the results are really true. It may only apply to patients who are able to have surgery after treatment with immunotherapy.
What does this mean for glioblastoma researchers?
It really changes our outlook on how to move forward. We need to design more studies that allow us to evaluate the effect of drugs on the tumor. Surgery may also need to be a more integral component of immunotherapy treatment.
What are the challenges of treating glioblastoma with immunotherapy?
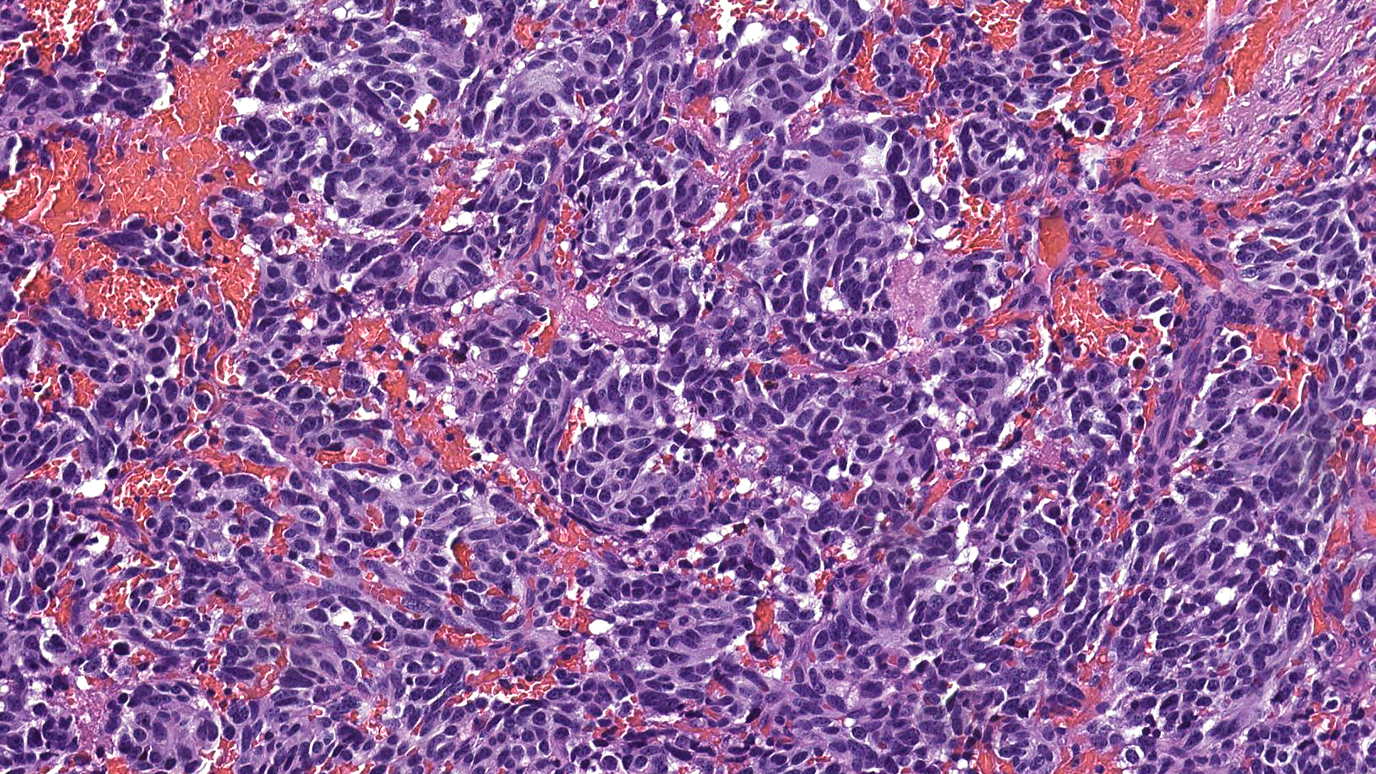
This study looked at an immune checkpoint inhibitor. To date, checkpoint inhibitors have been the most successful immunotherapy treatment for other cancers. Immune checkpoint inhibitors focus on T cells. The cancers where checkpoint inhibitors have been most successful, such as melanoma and non-small cell lung cancer, tend to have more T cells within the tumor than glioblastoma. This is one reason researchers have hypothesized that previous checkpoint inhibitor trials failed in glioblastoma.
Glioblastoma also contains many different types of cells, and a wide variety of immune cells. Because it’s such a complex disease, it’s hard to kill the tumor with any therapy that affects just one type of cell.
What other forms of immunotherapy are under study for glioblastoma and other brain tumors?
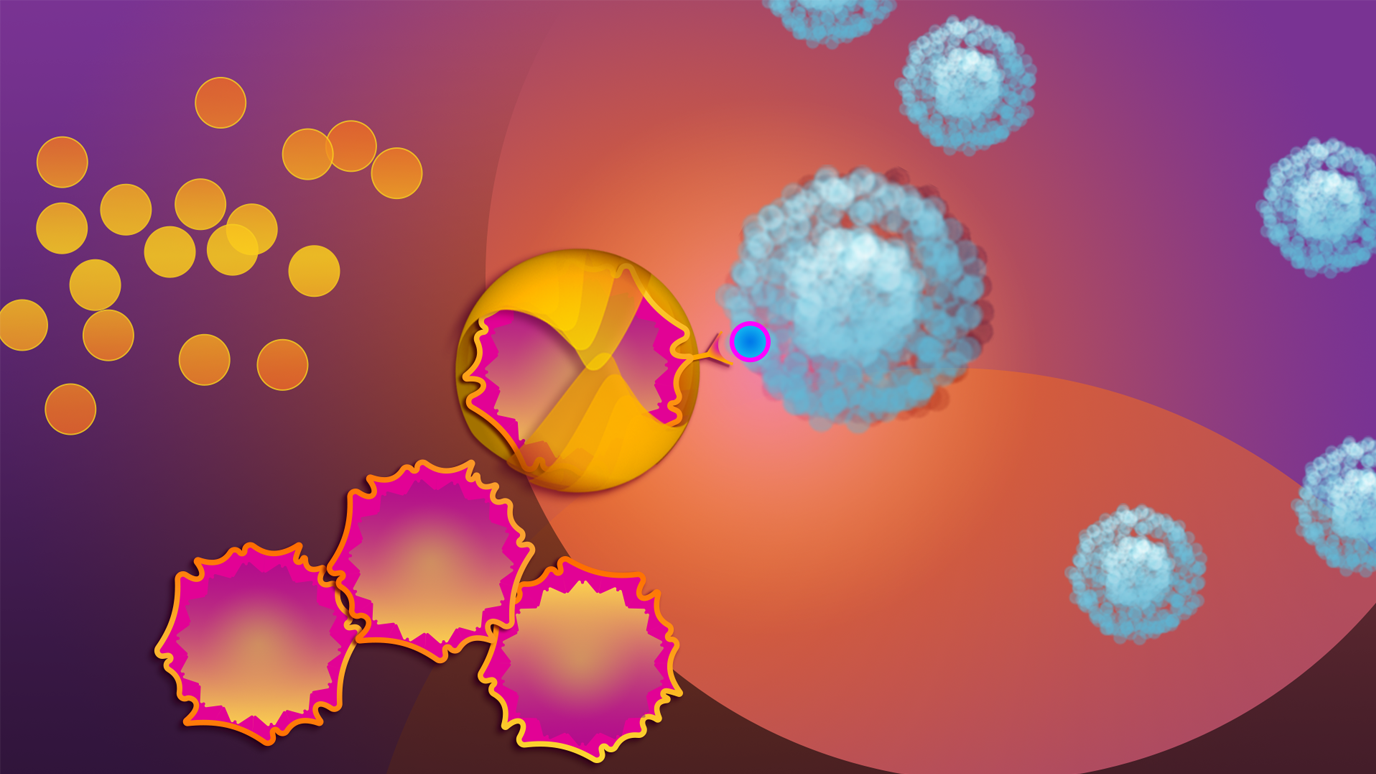
We’re actively investigating both checkpoint inhibitors and other types of immunotherapy for lower-grade gliomas, brain metastasis and pediatric brain tumors. For example, a drug developed at MD Anderson to target the STAT3 pathway, which helps cancer cells avoid the immune system, recently entered a Phase I clinical trial for recurrent malignant gliomas and melanoma brain metastasis. Another Phase I clinical trial is using NK cells, a different type of immune cell, for advanced pediatric brain tumors. And now we’re finding that viral therapies, like Delta-24-RDG, may actually work in part by triggering an immune response.
In the pre-clinical setting, our scientists are investigating immune “hubs” that keep the immune system from recognizing and attacking glioblastoma. We’re working to increase our understanding of how the immune system works both within tumors and in the microenvironment surrounding the tumor.
What should I do if I want to join a brain tumor immunotherapy clinical trial?
Clinical trials are considered for brain tumor patients at two points: 1) initial diagnosis and 2) recurrence. Talk to your doctor to learn what trials may be an option for you because each clinical trial has different eligibility requirements. See brain tumor clinical trials from MD Anderson’s Neuro-Oncology and Neurosurgery departments here and all clinical trials at MD Anderson here.
Is there anything else you want newly diagnosed glioblastoma patients and their families to know?
We recognize there’s still a long way to go to improve survival for all glioblastoma patients, but we’re hopeful that immunotherapy will provide a way forward. Know that we are so grateful to each and every person who participates in a clinical trial – we can’t make progress without you.
Request an appointment at MD Anderson online or by calling 1-855-948-6381.
Related Cancerwise Stories

It really changes our outlook on how to move forward.
John de Groot, M.D.
Physician