- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (160)
- Colon Cancer (166)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (98)
- Tonsil Cancer (30)
- Uterine Cancer (82)
- Vaginal Cancer (18)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (632)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (920)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (606)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (322)
- Symptoms (182)
- Treatment (1786)
A next-generation treatment for bile duct cancer
3 minute read | Published October 22, 2023
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on October 22, 2023
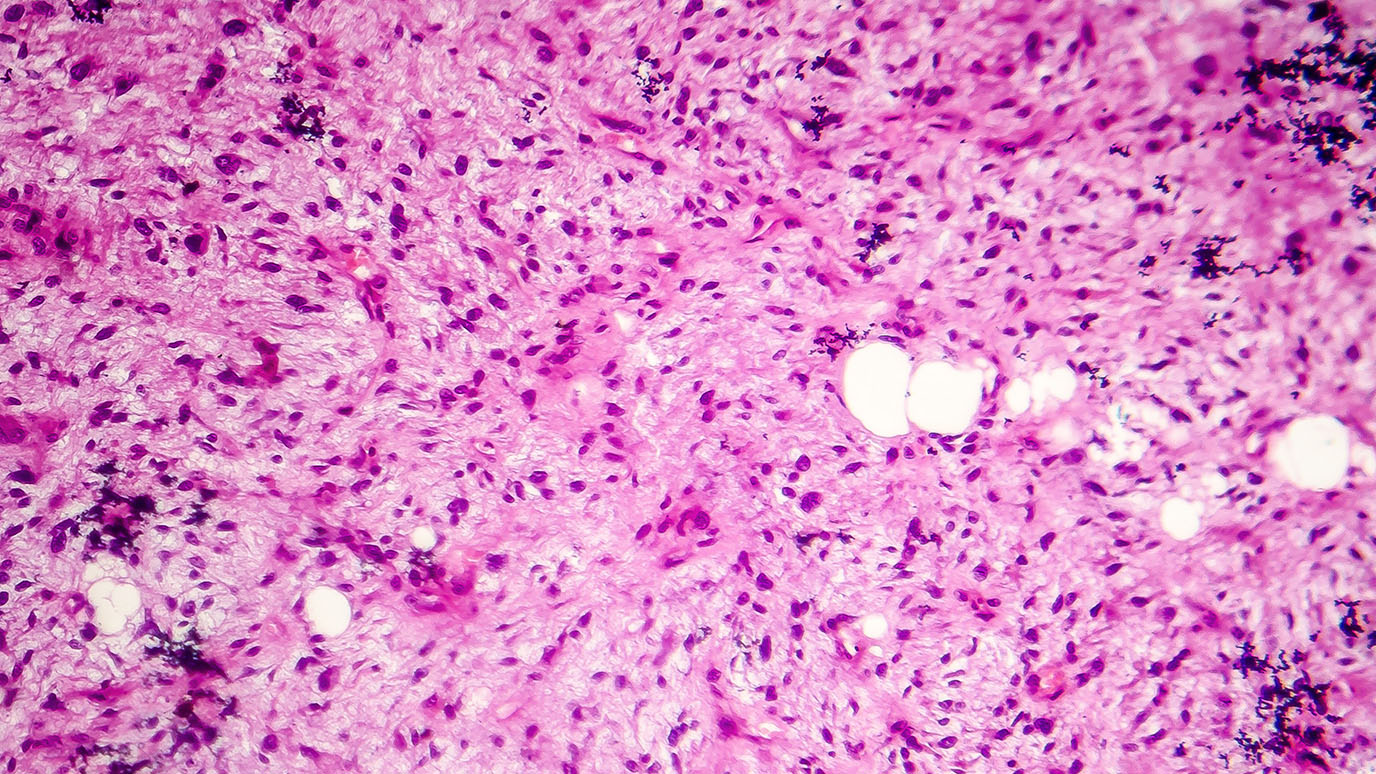
For patients with cholangiocarcinoma, or bile duct cancer, the first line of treatment often includes standard cancer treatments, such as surgery, chemotherapy and radiation therapy. However, in the last few years, oncologists have found that there may be a better option for patients whose cancer has a mutation in the fibroblast growth factor receptor (FGFR).
FGFR inhibitors, in combination with standard treatments, have extended the lives of many with this disease. However, these drugs often stop working after six to eight months.
“These drugs work very well for a while, but resistance is inevitable,” says gastrointestinal medical oncologist Milind Javle, M.D.
Now, a new type of FGFR inhibitor may allow patients to live longer without their disease progressing.
Javle will present Phase II clinical trial results at the 2023 European Society for Medical Oncology (ESMO) Congress.
The latest treatment for cholangiocarcinoma
The drug being studied in the clinical trial, tinengotinib, is an example of a next-generation FGFR inhibitor because it binds to the FGFR2 in a unique way.
This approach does seem to extend survival among patients, especially among those who initially responded to an FGFR inhibitor — the clinical trial showed a median progression-free survival of seven months. This means half the patients went longer without their cancer progressing, and half shorter. Even though seven months may not seem like a lot, it could be meaningful, Javle says, because in some cases, the patients can survive for years.
The science behind how tinengotinib works
FGFR inhibitors often stop working after a few months because the cancer acquires new genetic mutations — it essentially evolves — to become resistant to the medication. These cancer cells are then able to tolerate the original FGFR inhibitor.
Tinengotinib, on the other hand, has a unique binding mechanism away from the ATP binding pocket that enables it to target even newly resistant cancer cells. It overcomes acquired resistance by targeting FGFR2 kinase domain mutations. Essentially, by inhibiting a number of different kinases (a particular type of enzyme important for cell growth), the drug targets the spread of the cancer cells with their acquired resistant mutations.
These new treatments highlight the need to better understand each patient’s cancer genetics at different points in time.
“Genomic profiling with next-generation sequencing is really important,” Javle says. “And because the cancer evolves, the genomic profiling of the tumor should be repeated after therapy to see if new changes have been acquired.” This can be done with a simple blood test called a liquid biopsy.
Studying the safety and effectiveness of tinengotinib in patients
In the clinical trial, there were three groups of patients: those for whom the FGFR inhibitor worked for some time then stopped working, those for whom the FGFR inhibitor never worked, and those whose cancer didn’t have any FGFR mutations. When beginning the study, 97% had stage IV disease. About half of the patients had already tried an FGFR inhibitor.
One of the main things Phase II clinical trials consider is the drug's safety. Although drug-related adverse events occurred in more than 80% of patients, they were all manageable, and there were no deaths related to the drug. Most of these side effects were mild and went away after treatment ended.
There was good news about the drug’s effectiveness as well: Overall, the response rate was about 20%, and the disease control rate was almost 75%. For patients who had previously tried an FGFR inhibitor, the response rate was 34%, and the disease control rate was 90%.
“These are respectable figures for a disease for which there are no current options,” Javle says. “The study showed notable clinical benefit for cholangiocarcinoma patients with acquired resistance to prior FGFR inhibitors.”
Future research seeks to provide more treatment options
The next step is a worldwide randomized Phase III clinical trial, led by MD Anderson, which is already open for enrollment at some centers. This study will further evaluate tinengotinib in cholangiocarcinoma patients with alterations in FGFR2 and whose disease has progressed after receiving one of the first-generation FGFR inhibitors.
“We are hoping that this work will lead to subsequent approval of therapeutic options for patients who have stopped responding to the first-line treatments,” Javle says.
Request an appointment at MD Anderson online or by calling 1-877-632-6789.
We are hoping that this work will lead to subsequent approval of therapeutic options for patients who have stopped responding to the first-line treatments.
Milind Javle, M.D.
Physician