- Diseases
- Acoustic Neuroma (16)
- Adrenal Gland Tumor (24)
- Anal Cancer (70)
- Anemia (2)
- Appendix Cancer (18)
- Bile Duct Cancer (26)
- Bladder Cancer (74)
- Brain Metastases (28)
- Brain Tumor (234)
- Breast Cancer (726)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (164)
- Colon Cancer (168)
- Colorectal Cancer (118)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (14)
- Kidney Cancer (130)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (6)
- Neuroendocrine Tumors (16)
- Oral Cancer (102)
- Ovarian Cancer (178)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (150)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (300)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (66)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (100)
- Tonsil Cancer (30)
- Uterine Cancer (86)
- Vaginal Cancer (18)
- Vulvar Cancer (22)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (22)
- Advance Care Planning (12)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (360)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (628)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (238)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (128)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (122)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (936)
- Research (390)
- Second Opinion (78)
- Sexuality (16)
- Side Effects (616)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (408)
- Survivorship (328)
- Symptoms (182)
- Treatment (1788)
7 questions about double-hit lymphoma, answered
BY Devon Carter
5 minute read | Published September 09, 2021
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on September 09, 2021
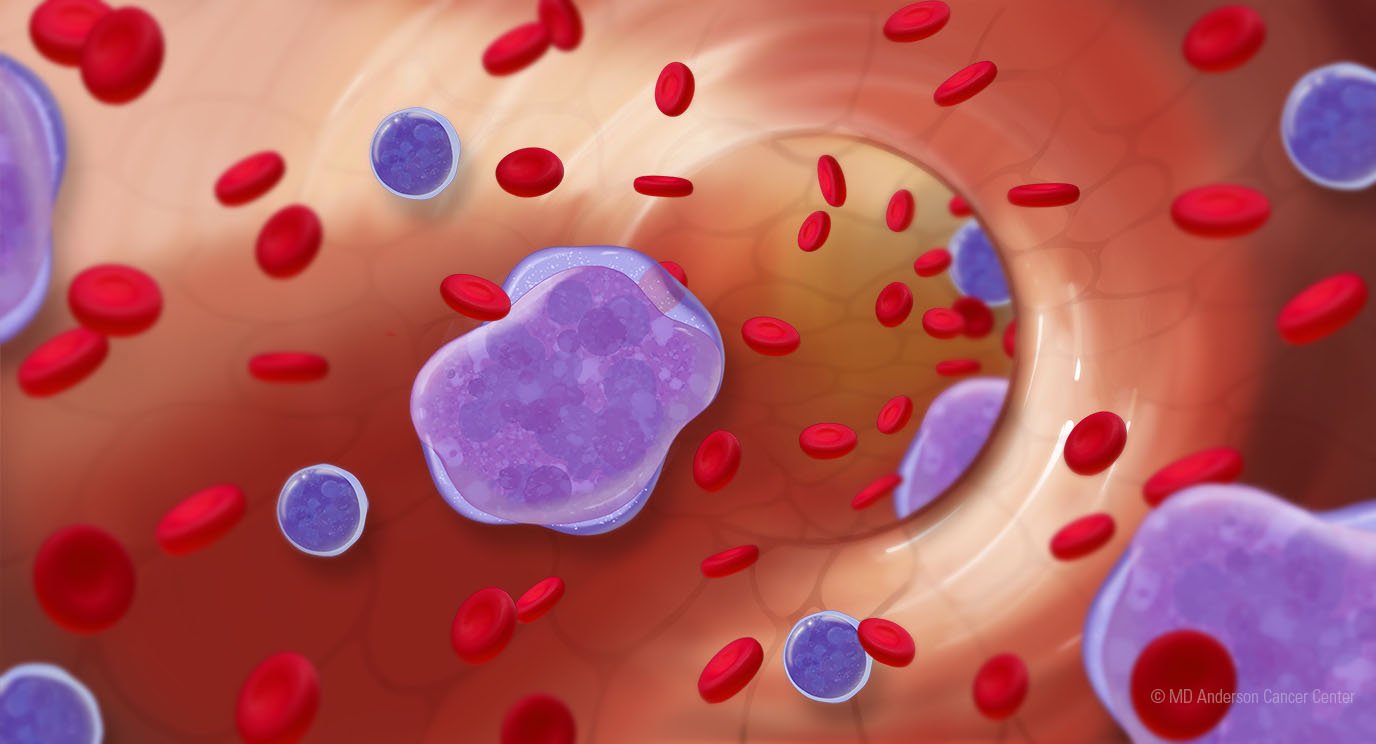
If you’ve never heard of double-hit lymphoma or you’re unfamiliar with the specifics of the disease, you’re not alone. This rare and aggressive subtype of diffuse large B-cell lymphoma (DLCBL) was first classified as a specific diagnosis in 2016.
But what sets it apart from other lymphomas, especially other types of diffuse large B-cell lymphoma? How is it diagnosed, and how is it treated?
To answer these questions, we spoke with lymphoma specialist Sairah Ahmed, M.D.
What is double-hit lymphoma?
Traditionally, diffuse large B-cell lymphoma (DLBCL) has been classified based on the risk of the cancer recurring. We considered a patient’s age, the extent of the disease, lab results and the patient’s overall health.
More recently, we’ve been able to improve our prediction of high-risk disease by looking at the presence of oncogenes through molecular profiling. Oncogenes are the instructions for when cells die, when they reproduce and how they carry out their function. These genes are very regulated and have a specific order, but when they rearrange – a process known as translocation – it can result in cancer.
In diffuse large B-cell lymphoma, the most common abnormalities involve the oncogenes BCL2, BCL6 and MYC. When there is a translocation of the oncogene MYC with either the rearrangement of BCL2 or BCL6, the diagnosis is double-hit lymphoma. At times, the MYC gene is translocated with both BCL2 and BCL6 rearrangements; this can be referred to as triple-hit lymphoma. These abnormal chromosomal changes are what define the diagnoses and set them apart from other lymphomas.
What is double-expressor lymphoma?
Double-hit lymphoma and double-expressor lymphoma are sometimes lumped into one subgroup, but they’re not the same. With double-expressor lymphoma, we’re able to see overexpression of MYC, BCL2 or BCL6 proteins, but they may or may not have translocation. The chromosomes don’t always rearrange like they do with double-hit lymphoma. That distinction is important because these diagnoses should be treated differently, too.
What are the symptoms of double-hit lymphoma?
This type of lymphoma usually makes people feel pretty sick. They may experience night sweats that require them to get up and change their bedding or lose weight without really trying. Often, patients may lose more than 10% of their body weight. They also commonly report frequent fevers, fatigue and pain in areas of their body they hadn’t previously experienced it.
Another sign to watch for is enlarged lymph nodes at the neck, under the arm or in the groin area. These swollen nodes are generally painless, but it’s important to talk to your doctor if you experience these symptoms for longer than two weeks.
How is double-hit lymphoma diagnosed?
Like we do with other types of lymphoma, we look at a patient’s blood cell counts and a bone marrow biopsy, as well as imaging results from PET scans and CT scans. To confirm the translocation of MYC with BCL2 and/or BCL6, we use a specialized technique called fluorescence in situ hybridization, commonly called FISH.
Double-hit lymphoma has an increased risk of spreading to the brain, so before starting treatment, patients often receive a lumbar puncture in the lower back to look for lymphoma cells in the fluid surrounding the brain.
How are double-hit and triple-hit lymphoma treated?
Although there are other chemotherapy options, the best and most commonly used one is an intensive regimen called dose-adjusted R-EPOCH. As with other regimens, patients need to be followed closely, but its side effects are manageable.
It’s given as an infusion through a port or a PICC line over three or four days. You can receive this chemotherapy as an inpatient or outpatient procedure, depending on how well you’re doing overall. As an outpatient, you’ll receive a portable pump that’s like a backpack, but you’ll still have to come in every day to switch out the chemotherapy drug. It’s also important to have a reliable caregiver who can call us or bring you in if something starts to feel off.
To help prevent lymphoma from spreading to the brain, you may also receive chemotherapy through a lumbar puncture. If we find lymphoma cells in the brain at diagnosis, we add different chemotherapy drugs to R-EPOCH to treat those cells.
Patients also used to receive an autologous stem cell transplant. But we’ve seen that if patients have a complete response to the chemotherapy, the stem cell transplant isn’t needed. Patients do just as well without a stem cell transplant if they receive the aggressive R-EPOCH therapy up front.
What are the treatment side effects?
With R-EPOCH, you’re at an increased risk of infection. To help manage that risk, patients often receive additional medications, such as antibiotics or a growth factor shot, which helps boost your white blood cells and strengthen the immune system.
Other common side effects include hair loss, nausea, diarrhea and low blood count. Fortunately, we have good medications that can offer you relief from nausea and bowel changes. And two to three months after completing treatment, you can expect your energy level to return to normal and to see your hair grow back.
What if I have a relapse? How is it treated?
Unfortunately, if lymphoma comes back, it’s hard to get under control again. If the disease has already responded once to chemotherapy, our first plan is usually more chemotherapy and an autologous stem cell transplant. But if that doesn’t work, we have more options.
A newer treatment called CAR T cell therapy has changed the way that we treat lymphoma and can be an option that may provide a cure for a subset of patients. Several emerging therapies, including new chemotherapies as well as immunotherapies and targeted therapies, have also shown to be able to treat double-hit lymphoma.
Although double-hit lymphoma is rare, we’ve come a long way understanding it better. I’m hopeful for the future, and I want patients to be, too.
Request an appointment at MD Anderson online or by calling 1-855-838-3785.
Related Cancerwise Stories
Although this disease is rare, we've come a long way in understanding it better.
Sairah Ahmed, M.D.
Physician