Image Guided Cancer Therapy Research (IGCTR) Program
Founding Director:
Kristy K. Brock, Ph.D., DABR, FAAPM, FASTRO, FAIMBE
Professor, Imaging Physics
Professor, Radiation Physics
- Departments, Labs and Institutes
- Research Centers and Programs
- Image Guided Cancer Therapy Research Program
The University of Texas MD Anderson Cancer Center has spearheaded an initiative designed to leverage advanced imaging techniques so that physicians can see, track and monitor tumor and normal tissue conditions in near-real time.
The Image Guided Cancer Therapy (IGCT) Research Program is designed to accelerate the development of innovative new approaches that are more effective, less invasive and more economical, as well facilitate commercialization of developed technologies, to improve cancer care at MD Anderson and around the world.
Using imaging to guide treatment procedures provides a valuable capability to accurately focus therapy to target the tumor, spare healthy tissue and dramatically reduce the risk of side effects. Further, we are finding new ways to use imaging to guide cancer therapy to make procedures more minimally invasive.
The ultimate of the program is simple: local-regional tumor control and reduced toxicities through research and development of advanced image-guided focal cancer treatment.
The program helps strategically aggregate faculty interested in this research from Diagnostic Imaging, Surgery and Radiation Oncology. The intention is to empower multidisciplinary teams of physicians and scientists to address the clinical challenges and technology barriers using resources of the program to drive the translation of innovative science directly to patient care.
IGCT T32 Program
We are accepting applications from those with a Ph.D. and/or M.D. Learn more about the program.
Program Updates
The FY23 IGCT Program Update is now available.
View the FY2023 IGCT Program Update
View the FY2022 IGCT Program Update
View the FY2021 IGCT Program Update
View the FY2018–FY2020 IGCT Triennial Program Update
Donate
Your gift will help us transform image-guided focal therapy to directly improve outcomes for cancer patients treated at MD Anderson and around the world.
Our resources and equipment enable physicians to monitor tissue conditions using non-invasive measures. They include:
BrainSUITE™ iMRI is the first intra-operative MRI and surgical navigation system in the world. We are actively working to improve the accuracy of image integration by modeling the anatomical changes during the surgical intervention.
MR-LINAC is the first MRI integrated with radiation therapy delivery in the United States. Our research will leverage this unique integration of MRI with radiotherapy to improve our understanding of radiation toxicity and enable an advanced level of personalized treatment.
MIYABI Suite is a hybrid operating/interventional room equipped with angiography and CT scanning capability. Innovative research is investigating the translation of biomechanical models of the liver to improve the targeting of liver tumors during focal ablation
Correlative Pathology is technology to allow validation of novel imaging with pathology results. We are developing techniques to better understand the effect of novel breast cancer treatments through innovative imaging validated through precise correlation to pathology.

Strategic Goals
We're focused on developing new imaging methods and improving the way current imaging techniques are used through the following strategic goals and initiatives:
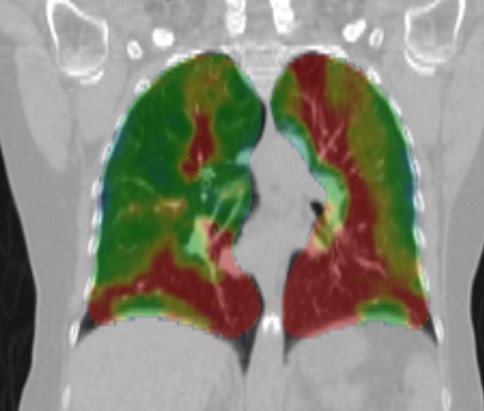
Develop and validate novel imaging to identify and target the tumor while avoiding normal tissue
- Use advanced imaging approaches to better resolve tumor and normal tissue anatomic relationships, tumor heterogeneity, biology, and function for better tumor targeting.
- Understand normal tissue function and response to therapy.
- Validate imaging phenotypes by correlative pathology.
- Develop novel imaging agents for both planning and intervention in collaboration with The Center for Biomedical Imaging (CABI).
Advance in-room integration of imaging to reduce uncertainties in executing the planned intervention
- Rapid imaging for ‘real-time’ interventional updates and guidance.
- Anatomical modeling to integrate planning images into the interventional space.
- Intelligent visualization to inform clinician of the current status.
- Establish infrastructure to accurately understand delivered local therapy and outcomes. of the patient.
Demonstrate clinical impact through documentation of improved local control and quality of life
- Improve communication of information and data between clinicians and interventional platforms.
- Prospectively collect delivered intervention and outcomes data.
- Enable streamlined data sharing to promote big data science.
- Optimize use and allocation of technology and resources.
Provide mentorship in developing multi-disciplinary research and grant writing
The Center for Advanced Biomedical Imaging (CABI)
Combining the collaborative clinical and scientific expertise of GE Health Care, UT Health Science Center (Houston) and MD Anderson
