Diet soda and cancer risk: What you should know
Diet soda has few, if any, calories. So, you may think it’s a healthier, waist-shrinking alternative to regular soda. But that’s not the case.
Research shows that people who drink diet beverages consume significantly more calories from food than people who drink sugar-sweetened beverages, like regular soda. These extra food calories can add up to a higher number on your bathroom scale. And people with obesity or higher weights are at increased risk for more than 10 types of cancer.
Invasive ductal carcinoma: 6 things to know about this common breast cancer
What can a pathology report tell you?
Gynecologic oncologist: Why I’m passionate about cancer care at MD Anderson
Diet soda and cancer risk: What you should know
What are the symptoms of liposarcoma?
Personalized treatment helps retired physician overcome dual cancer diagnoses
|
$entity1.articleCategory
|
|---|
|
$entity2.articleCategory
|
|
$entity3.articleCategory
|
|
$entity4.articleCategory
|
|
$entity5.articleCategory
|
|
$entity6.articleCategory
|
Find stories by topic
Find out everything you need to know to navigate a cancer diagnosis and treatment from MD Anderson’s experts.
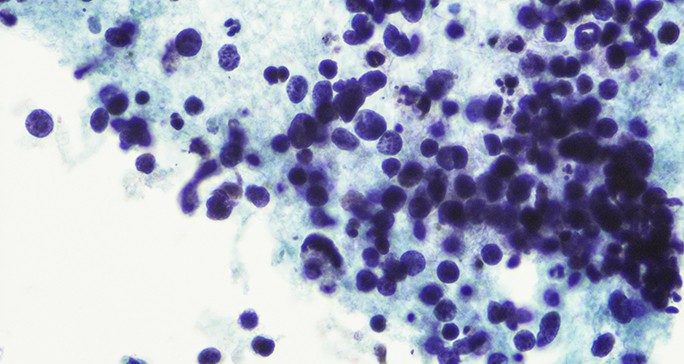
What can a pathology report tell you?
April 10, 2025
What are the symptoms of liposarcoma?
April 08, 2025
Cancer treatment side effect: Muscle cramps
April 03, 2025
What types of cancer can cause itchy skin?
March 24, 2025
Read inspiring stories from patients and caregivers – and get their advice to help you or a loved one through cancer.
Music to a mother’s ears: Awake craniotomies bring musicians together
February 24, 2025
Art Space volunteer draws inspiration from young friend
January 31, 2025
Get MD Anderson experts’ advice to help you stay healthy and reduce your risk of diseases like cancer.
Diet soda and cancer risk: What you should know
April 09, 2025
How to get your heart rate up
April 04, 2025
What happens when you overeat?
April 01, 2025
How to make colonoscopy prep better
March 31, 2025
Negative effects of vaping on teens
March 28, 2025
How to avoid injury when starting a new exercise routine
March 19, 2025
How to clean your ears safely: Tips to avoid harm
March 17, 2025
Learn how MD Anderson researchers are advancing our understanding and treatment of cancer – and get to know the scientists behind this research.
How non-scientists are helping cancer researchers
February 21, 2025
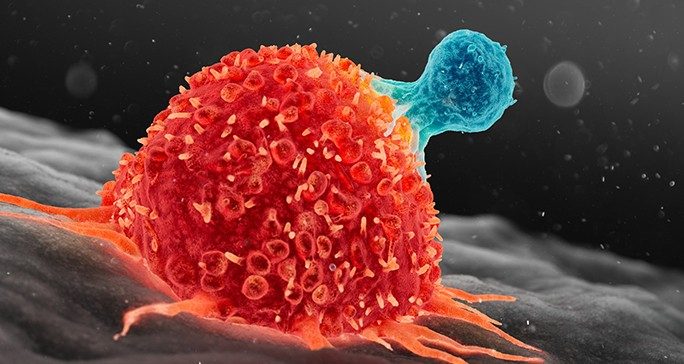
4 questions with immunology researcher Susan Bullman
February 04, 2025
4 questions for mathematical oncologist Heiko Enderling, Ph.D.
January 28, 2025
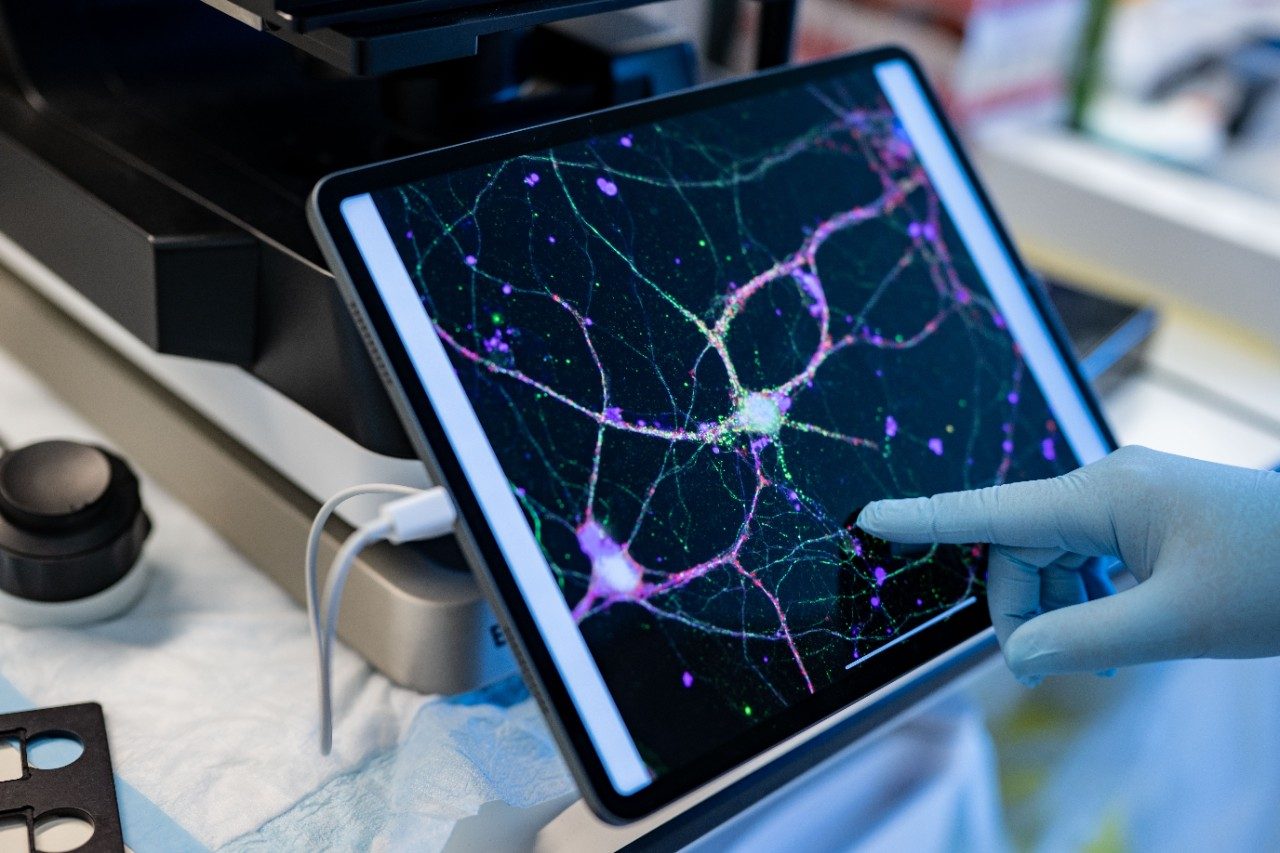
Committed to making cervical cancer screening easier
January 08, 2025
11 new research advances from the past year
December 19, 2024
Finding hope for cancer patients in ferroptosis research
December 12, 2024
Advances in small cell lung cancer classification
November 25, 2024
Exploring pancreatic cancer vaccines: What’s next?
November 21, 2024
Read insights on the latest news and trending topics from MD Anderson experts, and see what drives us to end cancer.
How to take medications properly: 6 questions, answered
February 28, 2025
Clinical Ethics Fellow passionate about improving patient care
February 27, 2025
Senior speech pathologist: Patients are my No. 1 priority
February 19, 2025
Motivated to do more for pediatric patients
February 18, 2025
Leukemia nurse fulfills promise to her late mother
February 17, 2025
Find out what inspires our donors to give to MD Anderson, and learn how their generous support advances our mission to end cancer.
Three cancer survivors raise funds to support Colorado patients
October 03, 2024
Inflammatory breast cancer survivor finds hope at MD Anderson
October 24, 2023