Ventilator-associated pneumonia incidents down to zero

For efforts that have led to reducing the incidence of ventilator-associated pneumonia (VAP) in its intensive care unit (ICU) to zero, MD Anderson received the Texas Hospital Association’s inaugural Bill Aston Award for Quality.
VAP is the most lethal health care-associated infection and increases ICU stays by up to 22 days and hospital stays by up to 25 days.
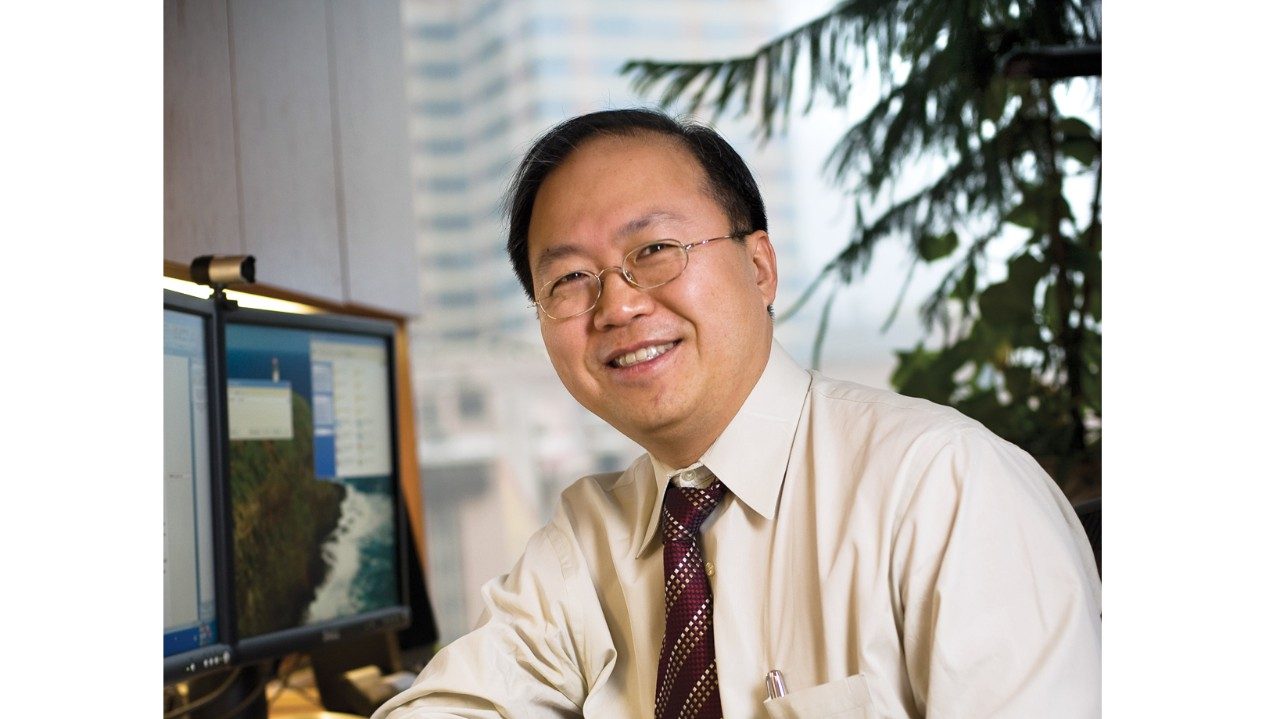
In 2002, Joseph Nates, M.D., joined MD Anderson and learned that the ICU’s VAP rate was 34.2 cases per 1,000 ventilator days, double the national average for trauma ICUs. The following year, he and his colleagues implemented aggressive multidisciplinary strategies to reduce the VAP rate. By 2009, that rate had dropped to zero.
“Many of the techniques we’re using today had not even been published when we started eight years ago,” says Nates, professor in the Department of Critical Care and medical director of the ICU.
“That’s why you have to keep learning and working on the problem. We haven’t eliminated the causes. If we don’t continue to work on the factors that lead to VAP, the infections will come back.
“The main reason for achieving a rate of zero for the past year is that we’ve been persistent. We have a cohesive and aggressive multidisciplinary team that consists of physicians, nurses, respiratory therapists and infection control specialists who work together toward this common goal.”