Positive thoughts helped adenoid cystic carcinoma survivor heal
When Tammy Ebbinghaus was diagnosed with adenoid cystic carcinoma of the nasal cavity in 2023, the timing couldn’t have been worse. She was a working single mother of three – one of whom was a senior in high school.
To make matters worse, her local doctor told her this type of cancer typically has a poor prognosis.
Acupuncture during cancer treatment: What to know
Positive thoughts helped adenoid cystic carcinoma survivor heal
What causes chemobrain? New insights
When should you worry about your menstrual cycle?
Questions to ask your doctor when transitioning to cancer survivorship care
|
Diagnosis & Treatment
|
|---|
|
Healthy Living
|
|
Healthy Living
|
|
Diagnosis & Treatment
|
|
Healthy Living
|
Find stories by topic
Find out everything you need to know to navigate a cancer diagnosis and treatment from MD Anderson’s experts.
Acupuncture during cancer treatment: What to know
June 05, 2025
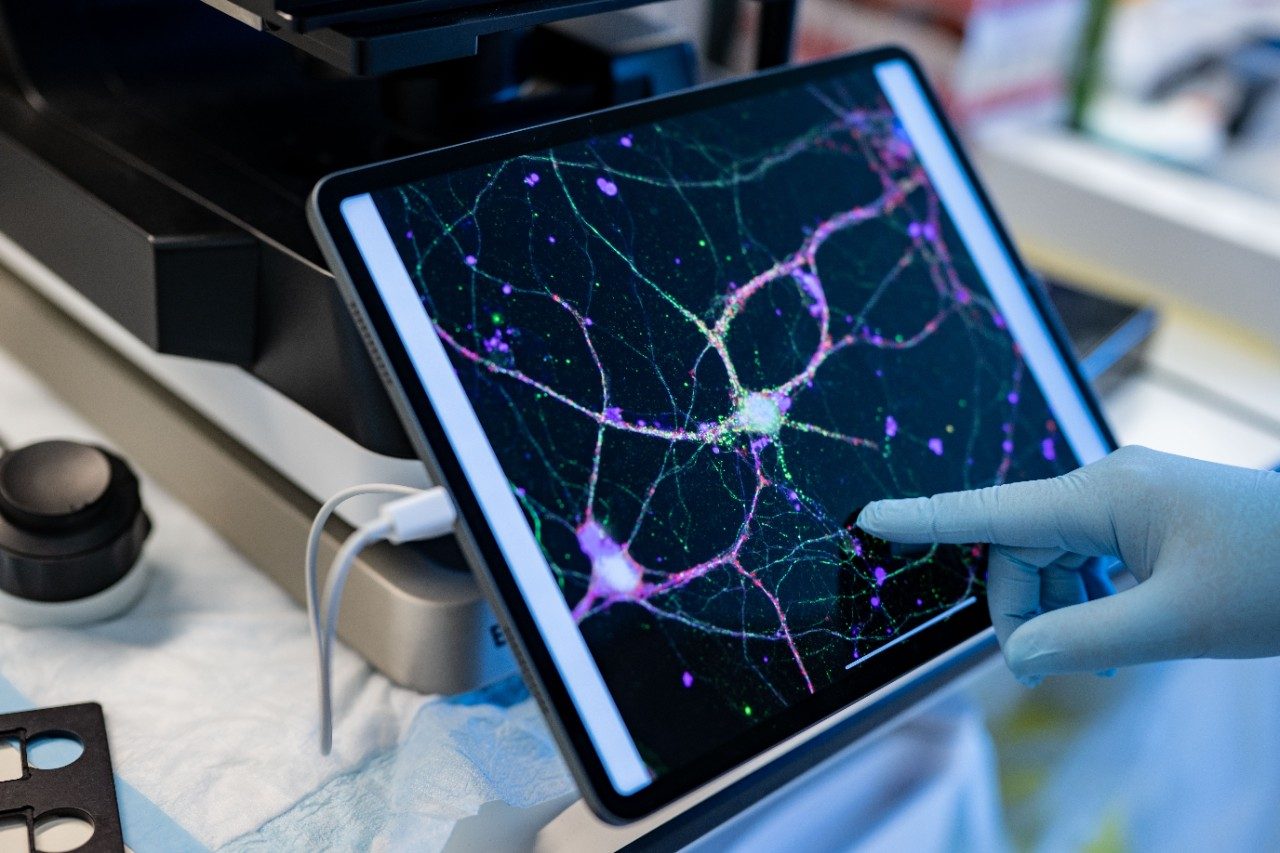
What causes chemobrain? New insights
June 03, 2025
When should you worry about your menstrual cycle?
June 02, 2025
7 things to know about myelofibrosis
May 27, 2025
Cancer of the jaw: 8 things to know
May 21, 2025
Which blood tests show cancer?
May 19, 2025
Read inspiring stories from patients and caregivers – and get their advice to help you or a loved one through cancer.
Mom's legacy lives on through fundraising for MD Anderson
April 28, 2025
Get MD Anderson experts’ advice to help you stay healthy and reduce your risk of diseases like cancer.
What SPF should I use?
May 23, 2025
Is raw milk safe?
May 16, 2025
How much caffeine is too much?
May 09, 2025
Learn how MD Anderson researchers are advancing our understanding and treatment of cancer – and get to know the scientists behind this research.
What causes chemobrain? New insights
June 03, 2025
Nutrivention: Food as medicine
May 28, 2025
5 emerging therapies presented at ASCO 2025
May 28, 2025
Top 5 MD Anderson abstracts at AACR 2025
April 25, 2025
Cell therapy: The evolution of the ‘living drug’
April 22, 2025
How non-scientists are helping cancer researchers
February 21, 2025
4 questions with immunology researcher Susan Bullman
February 04, 2025
4 questions for mathematical oncologist Heiko Enderling, Ph.D.
January 28, 2025
Read insights on the latest news and trending topics from MD Anderson experts, and see what drives us to end cancer.
Surgeon-scientist: ‘MD Anderson is unique’
May 15, 2025
Find out what inspires our donors to give to MD Anderson, and learn how their generous support advances our mission to end cancer.
Mom's legacy lives on through fundraising for MD Anderson
April 28, 2025
Three cancer survivors raise funds to support Colorado patients
October 03, 2024
Inflammatory breast cancer survivor finds hope at MD Anderson
October 24, 2023