Anesthesiology team focuses on the patient
MD Anderson's anesthesiology team evaluates, prepares and monitors every surgical patient, helps with special procedures, conducts research and emphasizes continued education.

Outside, a winter storm brings lashing winds and heavy rain to Houston. But in a surgical suite in MD Anderson’s Main Building, Nicolas Salazar is waking up in a hushed room.
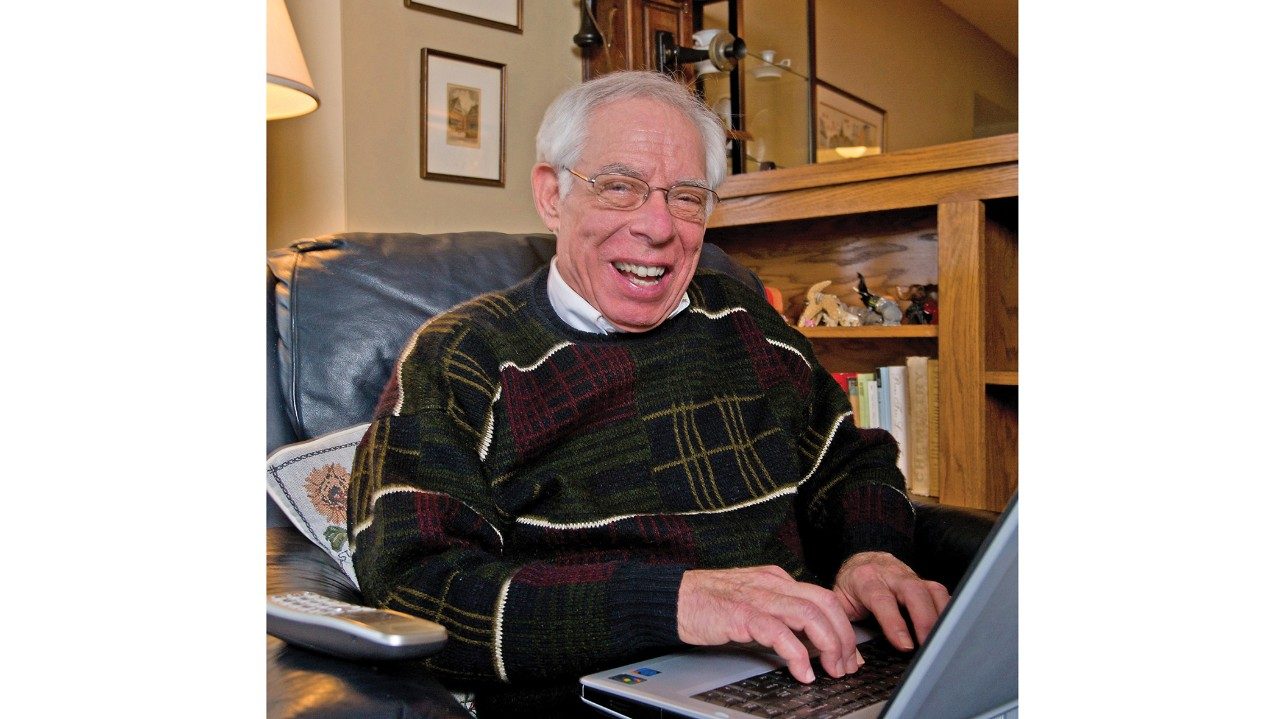
Coming out of anesthesia, he recognizes a kind face. David Ferson, M.D., professor in the Department of Anesthesia and Perioperative Medicine, smiles and gently clasps his hand. “You’re doing very well, Nicolas,” he says softly. “How do you feel?”
And with that, the most important member of the team for an awake craniotomy, in which the patient is conscious and talking for a portion of the surgery, has arrived.
‘Mapping the brain’ before removing the tumor
A 63-year-old insurance broker from Lima, Peru, Salazar is having his second brain surgery in as many months. Diagnosed late in 2011 with a central-brain glioblastoma, he underwent surgery in Lima in December. But the tumor was too difficult for the surgeons to remove, so Salazar and his family came to MD Anderson.
Lead neurosurgeon in Room 23 is Raymond Sawaya, M.D., professor and chair of the Department of Neurosurgery, assisted by fellow Lana Christiano, M.D. Before awakening the patient, they opened his skull to expose the brain.
Now they will “map” the brain, with Salazar’s help.
The awake procedure is ideal for certain brain tumors because the surgeon can trace the contours of the patient’s tumor to ensure that areas of the brain that control speech and movement are not involved. The goal is to excise as much of the tumor as possible without harming the patient’s ability to think, speak, move or reason.
In such a procedure, the anesthesia team first sedates the patient intravenously, then inserts a laryngeal mask airway for more precise control and delivery of the mix of anesthetics and sedatives. Once the patient is deeply asleep, the anesthesiologist administers a scalp block to completely numb the patient’s scalp for the surgery.
After the brain is exposed, the surgeon asks the anesthesiologist to awaken the patient so he or she can answer questions designed to demonstrate that speech faculties are intact.
Cultivating a new field: Anesthesiology Technologists Enhance OR Contributions

‘What do you see right now?’
Ferson shows Salazar a series of laminated flash cards, and Salazar names what he sees in Spanish and English. “Bull, toro. Train, tren. Shirt, camiso,” he says.
On the other side of the drape, Sawaya administers light electrical charges to areas of the brain. Salazar stumbles only once or twice, and Sawaya makes note of that.
Throughout, Ferson offers the patient ice chips, reassures him he’s doing well and clasps his hand. He focuses solely on Salazar and Sawaya. Behind him, James “Monie” Perry, certified registered nurse anesthetist (CRNA), keeps his eyes on the complex machines that indicate the patient’s vital signs.
Once the brain is mapped and the tumor is removed, Sawaya asks Ferson and Perry to put Salazar back to sleep for the rest of the operation.
Preparations, teamwork crucial to success
The day before surgery, Salazar, like all surgical patients at MD Anderson, has an appointment at the Anesthesia Assessment Center, where his case is evaluated and he and his family are educated about the awake craniotomy. The comprehensive evaluation also takes into account any pre-existing conditions that require special preparations before surgery.
The Department of Anesthesia and Perioperative Medicine consists of 65 anesthesiologists, 75 CRNAs and 20 anesthesia technicians and technologists, who make sure supplies are available and assist wherever needed.
Thomas Rahlfs, M.D., professor and chair of the department, is proud of his talented and productive team, which he believes is equal to the ever-growing demand for services.
In fact, he has big plans.

More time for research and education a priority
“We want to shift our faculty’s focus from strictly clinical to making time for research and education,” he says. “We actively recruit to ensure the staffing that makes that feasible.
“It’s a culture shift,” he acknowledges. “We’ve been 100% clinical, but we know how important it is to give our faculty time to pursue research or identify best practices.”
The department’s work would be impossible without the dedication and skill of scores of CRNAs. Garry Brydges, chief nurse anesthetist, has been with the department 10 years. The training and education required of his CRNA staff is rigorous, he says.
All have at least master’s degrees and have worked a minimum of one year in an intensive care unit (ICU) before entering training. This gives them exposure to a wide variety of complex cases.
“It’s one of those intangibles,” Brydges says. “ICU nurses carry out orders from a variety of specialists and master all the frontline lifesaving equipment. So those skills are honed even before anesthesia school.”
Induction (putting the patient to sleep) and emergence (waking up the patient) are the most critical parts of any anesthetic procedure, he says.
Samantha Sattari, a CRNA who’s been at the institution 11 years, describes the anesthesia team’s mission in a novel way. “We’re the pilots of the OR,” she says. “We make sure the patient takes off and lands safely.”
There’s an excitement — a thrill — to the work, she says. Even so, “When something unexpected happens, we stay calm.” Especially challenging are patients who have serious medical problems or devices such as pacemakers. Fortunately, the knowledge gathered in the pre-surgery assessment allows for preparation.
“With really sick patients, we’re hyper-vigilant. But we’re a team with myriad helping hands,” Brydges says.

Experts ‘run the board’ with an eye to staffing, efficiency
Running MD Anderson’s 31 Main Building operating suites requires focus, collaboration, diplomacy and finesse. Not to mention a giant white board and an online tool to keep track of OR capacity.
Front and center is the large white board listing all the surgical rooms, what’s happening in each and who’s staffing them.
Three days a week, Vijaya Gottumukkala, M.D., professor in the department, “runs the board.” He assures that staffing is adequate and rooms are used efficiently.
Gottumukkala also uses an online tool that tracks expected (and actual) demand hour by hour throughout the suites. Whoever is in charge updates the system constantly, and anyone trying to schedule a surgery can look at availabilities weeks and months ahead. Even so, there must be some leeway in the schedule for emergency surgeries, he says.
‘The fifth vital sign’
In addition to the neuroanesthesia required for awake craniotomies, the department supports other special anesthetic needs of surgeries or procedures.
For example, Marc Rozner, M.D., Ph.D., and Dilip Thakar, M.D., both professors in the department, are skilled at handling the considerations of patients with pacemakers who undergo all types of cancer surgeries. Under Rozner’s mentorship, three more anesthesiologists are preparing to take the International Board of Heart Rhythm Examiners’ Certification of Competency in Cardiac Rhythm Device Therapy exam. Together these five will make up an anesthesiologist-run perioperative pacemaker service, the first of its kind.
The department also has specialists in thoracic surgeries and in the Proton Therapy Center. Vivian Porche, M.D., is professor and medical director of anesthesia services at the center.
She’s seen incredible growth in the number of anesthetic procedures administered outside the operating room. These include anesthetics administered during interventional radiology and proton therapy procedures, as well as screening exams, such as endoscopies and colonoscopies. These procedures now make up more than half of the department’s cases.
“Our operation has grown so large,” she says. “And our No. 1 goal is that the anesthetics we offer are safe — as safe as in any OR. We consider pain the fifth vital sign — along with blood pressure, pulse, respiratory rate and temperature. We don’t want our patients to be in pain. They shouldn’t have to ‘tough it out.’”
Patient remembers experience
Two days after surgery, Salazar is recovering well in the hospital. All three of his children — son Nicolas and daughters Anali and Andrea — are now with him and his wife, Milagros.
He remembers being awake during surgery. He recalls speaking to Milagros and Anali by phone from the operating room, assuring them he was in good hands and in no pain.
Anali says that in the anesthetic assessment before surgery, Ferson asked her father whether he ever became angry or disruptive when he drank. This is relevant because those who have a history of being combative under the influence of alcohol might react the same way when awakened during surgery.
Salazar assured Ferson that he’s happy and pleasant when he drinks.
Andrea, who arrived from Vancouver, B.C., after the surgery, laughs. “He’s very nice — and very talkative,” she says.
And how has her father been since his incredible experience?
“He’s been hungry,” Andrea says. “Oh! And he thinks he speaks better English now — after the surgery.”
The family laughs and looks at Nicolas, who nods and smiles.