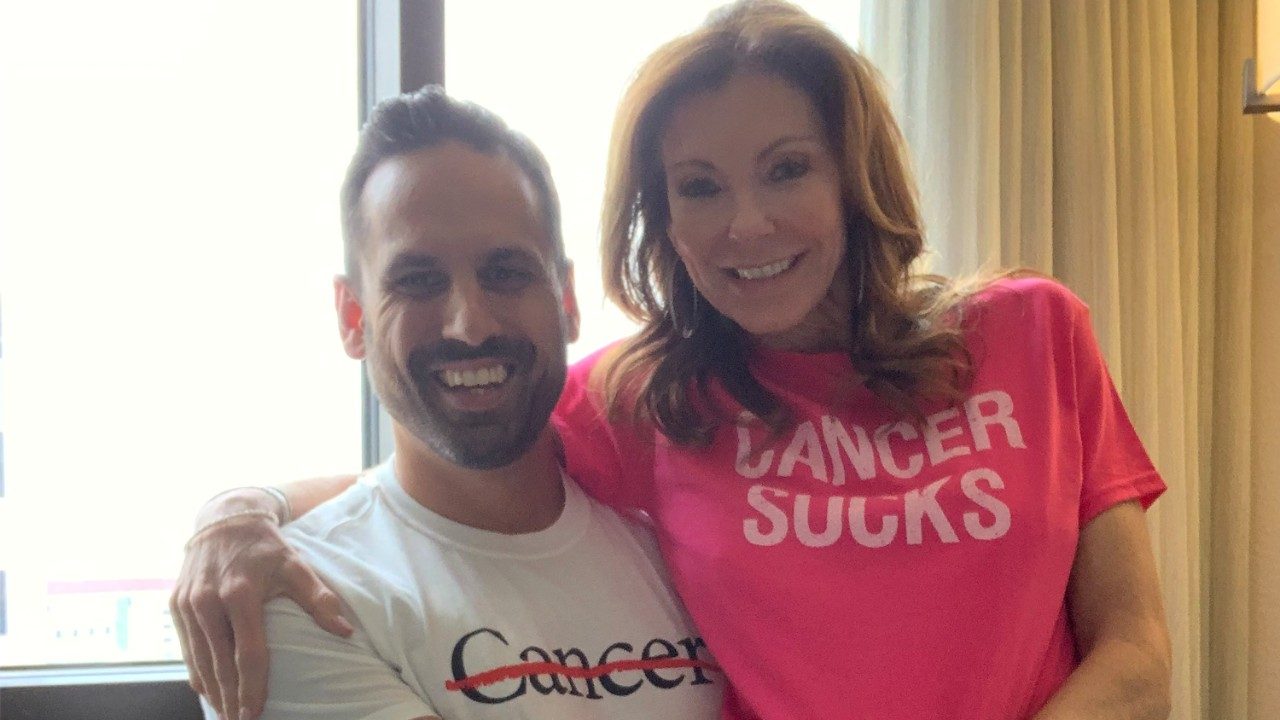
Young adult cancer pre-vivor: Why I had my stomach removed at age 25
Most people don’t realize you can live quite comfortably without a stomach. But I found that out first-hand in 2020, after learning I carry a genetic mutation called CDH1.
CHD1 dramatically increases your risk of developing both stomach cancer and lobular carcinoma, a type of breast cancer. The risk is so high for stomach cancer that doctors often recommend a total gastrectomy — or the complete surgical removal of your stomach — as a preventive measure. Once the stomach tissue is biopsied, pathologists often find that cancer cells are already present.
Cancer of the jaw: 8 things to know
Can sitting for too long really increase your cancer risk?
Young adult cancer pre-vivor: Why I had my stomach removed at age 25
Which blood tests show cancer?
Is raw milk safe?
Surgeon-scientist: ‘MD Anderson is unique’
|
$entity1.articleCategory
|
|---|
|
$entity2.articleCategory
|
|
$entity3.articleCategory
|
|
$entity4.articleCategory
|
|
$entity5.articleCategory
|
|
$entity6.articleCategory
|
Find stories by topic
Find out everything you need to know to navigate a cancer diagnosis and treatment from MD Anderson’s experts.
Cancer of the jaw: 8 things to know
May 21, 2025
Which blood tests show cancer?
May 19, 2025
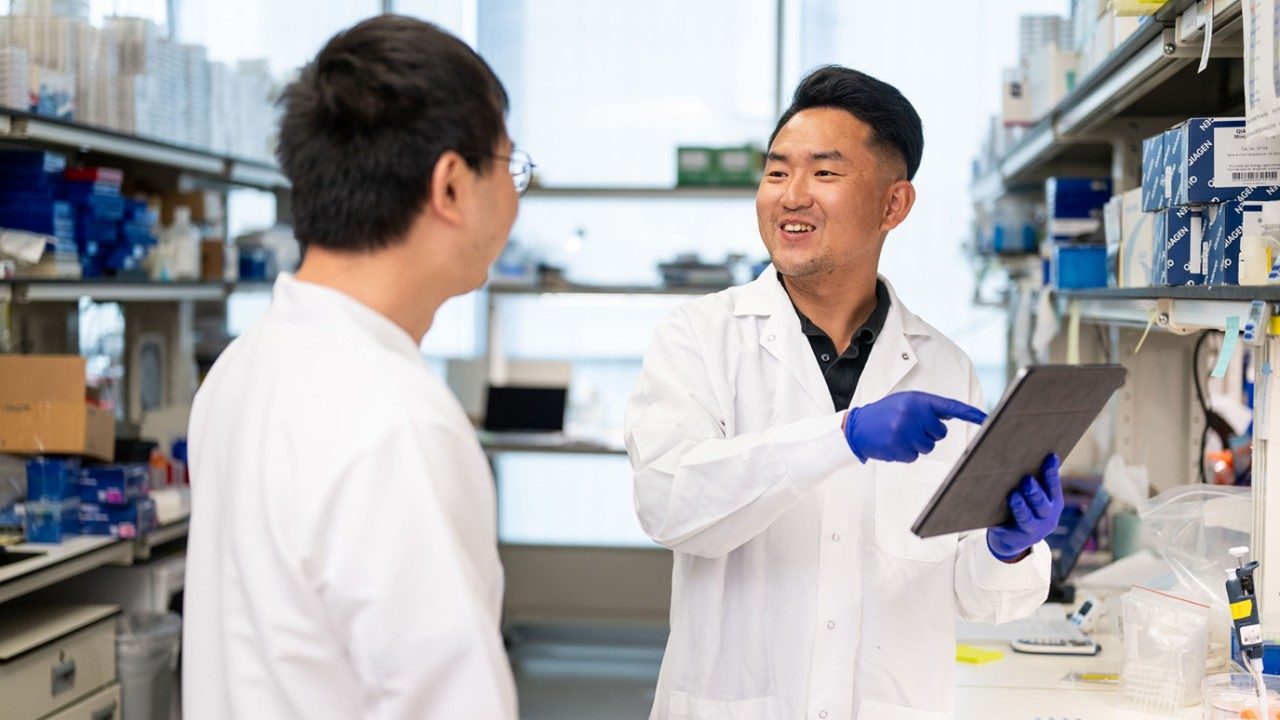
Surgeon-scientist: ‘MD Anderson is unique’
May 15, 2025
What are polyps?
May 13, 2025
PET scans: What are they and what to expect
May 02, 2025
Read inspiring stories from patients and caregivers – and get their advice to help you or a loved one through cancer.
Mom's legacy lives on through fundraising for MD Anderson
April 28, 2025
Get MD Anderson experts’ advice to help you stay healthy and reduce your risk of diseases like cancer.
Is raw milk safe?
May 16, 2025
How much caffeine is too much?
May 09, 2025
Beef tallow benefits: Should you use it?
May 06, 2025
Do GMOs cause cancer?
May 01, 2025
Detoxes, cleanses and fasts: What you should know
April 29, 2025
Learn how MD Anderson researchers are advancing our understanding and treatment of cancer – and get to know the scientists behind this research.
Top 5 MD Anderson abstracts at AACR 2025
April 25, 2025
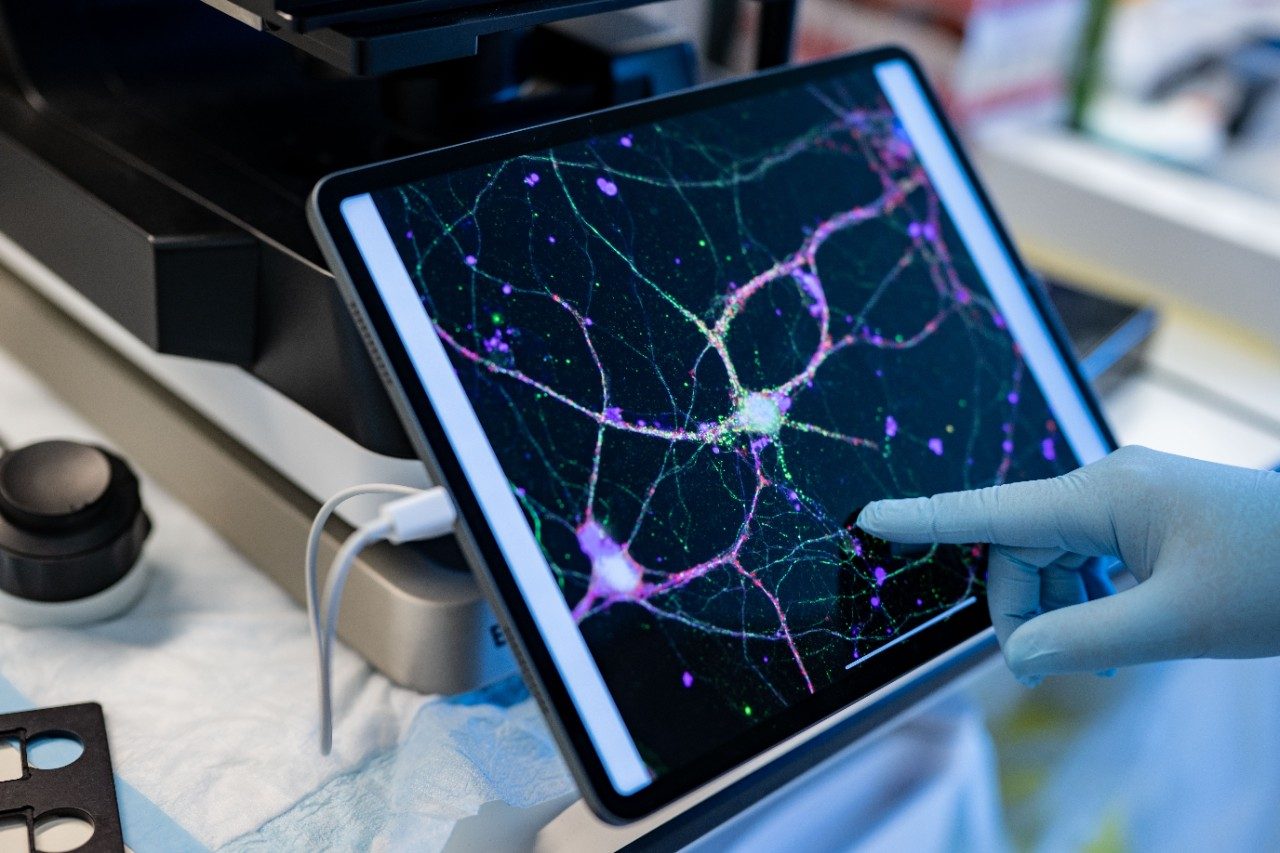
Cell therapy: The evolution of the ‘living drug’
April 22, 2025
How non-scientists are helping cancer researchers
February 21, 2025
4 questions with immunology researcher Susan Bullman
February 04, 2025
4 questions for mathematical oncologist Heiko Enderling, Ph.D.
January 28, 2025
Committed to making cervical cancer screening easier
January 08, 2025
11 new research advances from the past year
December 19, 2024
Finding hope for cancer patients in ferroptosis research
December 12, 2024
Read insights on the latest news and trending topics from MD Anderson experts, and see what drives us to end cancer.
How to take medications properly: 6 questions, answered
February 28, 2025
Find out what inspires our donors to give to MD Anderson, and learn how their generous support advances our mission to end cancer.
Mom's legacy lives on through fundraising for MD Anderson
April 28, 2025
Three cancer survivors raise funds to support Colorado patients
October 03, 2024
Inflammatory breast cancer survivor finds hope at MD Anderson
October 24, 2023