- Diseases
- Acoustic Neuroma (14)
- Adrenal Gland Tumor (24)
- Anal Cancer (68)
- Anemia (2)
- Appendix Cancer (16)
- Bile Duct Cancer (26)
- Bladder Cancer (72)
- Brain Metastases (28)
- Brain Tumor (232)
- Breast Cancer (714)
- Breast Implant-Associated Anaplastic Large Cell Lymphoma (2)
- Cancer of Unknown Primary (4)
- Carcinoid Tumor (8)
- Cervical Cancer (158)
- Colon Cancer (166)
- Colorectal Cancer (116)
- Endocrine Tumor (4)
- Esophageal Cancer (44)
- Eye Cancer (36)
- Fallopian Tube Cancer (8)
- Germ Cell Tumor (4)
- Gestational Trophoblastic Disease (2)
- Head and Neck Cancer (12)
- Kidney Cancer (128)
- Leukemia (342)
- Liver Cancer (50)
- Lung Cancer (286)
- Lymphoma (278)
- Mesothelioma (14)
- Metastasis (30)
- Multiple Myeloma (100)
- Myelodysplastic Syndrome (60)
- Myeloproliferative Neoplasm (4)
- Neuroendocrine Tumors (16)
- Oral Cancer (100)
- Ovarian Cancer (172)
- Pancreatic Cancer (160)
- Parathyroid Disease (2)
- Penile Cancer (14)
- Pituitary Tumor (6)
- Prostate Cancer (146)
- Rectal Cancer (58)
- Renal Medullary Carcinoma (6)
- Salivary Gland Cancer (14)
- Sarcoma (238)
- Skin Cancer (296)
- Skull Base Tumors (56)
- Spinal Tumor (12)
- Stomach Cancer (64)
- Testicular Cancer (28)
- Throat Cancer (92)
- Thymoma (6)
- Thyroid Cancer (96)
- Tonsil Cancer (30)
- Uterine Cancer (80)
- Vaginal Cancer (16)
- Vulvar Cancer (20)
- Cancer Topic
- Adolescent and Young Adult Cancer Issues (20)
- Advance Care Planning (10)
- Biostatistics (2)
- Blood Donation (18)
- Bone Health (8)
- COVID-19 (362)
- Cancer Recurrence (120)
- Childhood Cancer Issues (120)
- Clinical Trials (630)
- Complementary Integrative Medicine (22)
- Cytogenetics (2)
- DNA Methylation (4)
- Diagnosis (232)
- Epigenetics (6)
- Fertility (62)
- Follow-up Guidelines (2)
- Health Disparities (14)
- Hereditary Cancer Syndromes (126)
- Immunology (18)
- Li-Fraumeni Syndrome (8)
- Mental Health (116)
- Molecular Diagnostics (8)
- Pain Management (62)
- Palliative Care (8)
- Pathology (10)
- Physical Therapy (18)
- Pregnancy (18)
- Prevention (916)
- Research (392)
- Second Opinion (74)
- Sexuality (16)
- Side Effects (604)
- Sleep Disorders (10)
- Stem Cell Transplantation Cellular Therapy (216)
- Support (402)
- Survivorship (320)
- Symptoms (182)
- Treatment (1786)
Chemotherapy/immunotherapy combination thwarts glioblastoma in pre-clinical research
4 minute read | Published March 30, 2020
Medically Reviewed | Last reviewed by an MD Anderson Cancer Center medical professional on March 30, 2020
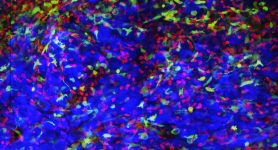
Triple combination therapy kills glioblastoma in mice by putting an “eat me” signal to the immune system on the surface of the brain tumor cells, blocking an offsetting “don’t eat me” signal and protecting a cancer-killing immune response launched by the combination.
The brain tumor treatment, as reported in Nature Communications, more than doubled median survival of mice treated with all three drugs, compared to those treated with only two of the drugs.
The key is using chemotherapy to expose tumors to phagocytosis -- being engulfed and destroyed by innate immune cells that also present antigens from cancer cells to T cells to launch an adaptive immune attack, explains research leader Betty Y.S. Kim, M.D., Ph.D., associate professor of Neurosurgery.
“This combination therapy is ready for clinical trials against both blood malignancies and solid tumors,” Kim says.
All three types of drug are available for human clinical trials:
- the chemotherapy temozolomide, approved for glioblastoma;
- antibodies to block CD47, a “don’t eat me” signal on cancer cells, presently in development;
- and immunotherapy drugs that block the PD-1 immune checkpoint on T cells, freeing them to attack tumors, which are approved for other cancers but ineffective alone against glioblastoma.
New impact for temozolomide
Temozolomide is an alkylating agent that kills cells by attaching methyl groups to DNA and is approved for use in glioblastoma. Kim and her team, working in Neurosurgery at the Mayo Clinic in Jacksonville, Florida, before she came to MD Anderson in 2019, discovered another important aspect of the chemotherapy.
“Temozolomide causes stress to the endoplasmic reticulum, a compartment in cells that processes proteins,” Kim says. This stress causes the endoplasmic reticulum to launch the protein calreticulin (CRT) to the cell surface.
“CRT, on the cell membrane, is an ‘eat me’ signal for macrophages,” Kim says. The team found increased phagocytosis of tumor cells when CRT is on the surface.
Blocking “don’t eat me” signal
Analyzing mouse and human glioblastoma lines, Kim and colleagues found heavy expression on the cell surface of CD47, which sends a conflicting signal to immune macrophages: “don’t eat me.”
Blocking CD47 alone did not prolong survival in mice.
When the team combined temozolomide with an antibody to block CD47, the combination increased phagocytosis by antigen-presenting macrophages and cleared tumor cells in cell lines. But it provided a modest median survival benefit in mice of about 10 to 15 additional days over either drug individually.
Calling those results “good but not amazing,” Kim and colleagues examined the impact of the combination on adaptive immunity.
Protecting adaptive immune response
A series of experiments showed that temozolomide and anti-CD47 increased antigen cross-presentation by the antigen-presenting macrophages that were eating tumor cells. Blocking expression of the CRT “eat me” signal negated this effect.
They also found the combination increased antigen-priming of T cells and produced more CD8 effector and memory T cells. The key pathway in this process on antigen-presenting cells was activation of cytosolic DNA-sensor stimulator interferon genes (STING). Treatment with the combination increased infiltration of tumors by cell-killing CD8+ effector T cells and CD4 helper T cells.
Depleting CD8+ effector T cells with an antibody nearly completely eliminated the anti-tumor effect of the combination therapy.
Further analysis showed increased expression of immune T cell checkpoint PD-1 and its ligand, PD-L1, in extracted tumors, promoting resistance to the adaptive immune response launched by the combination.
Treating mice with temozolomide, anti-CD47 and an anti-PD-1 checkpoint inhibitor resulted in a major increase in survival, with 55% of the triple-combination mice surviving beyond 80 days compared to 38 day median survival for the double combination.
Most of the adaptive immunotherapy research was conducted at MD Anderson.
Potential in other cancers
One of the paper reviewers asked the team about using other types of chemotherapy to induce the translocation of the CRT “eat me” signal to the cell surface.
They used the chemotherapy cisplatin with anti-CD47 antibody against a breast cancer line. They found 48 hours of treatment with the combination enhanced CRT translocation to the cell membrane, induced endoplasmic reticulum stress and increased antigen-presenting cell phagocytosis of the tumor cells.
“So it appears temozolomide is not unique in how it stresses cells,” Kim says. “All harsh chemotherapy in cancer treatment is taken to the maximum dose, killing rapidly-dividing cells with substantial side effects. This works for a while, then the cancer comes back.”
She adds, “Using this immune approach, activating cell-killing T cells and creating memory T cells, the immune system can provide long-term surveillance of tumor re-growth.”
PD-1 and other checkpoint blockade drugs have not succeeded against glioblastoma, probably due to a lack of T cells in the tumors. Glioblastomas contain lots of macrophages though, Kim notes, but many are not playing an anti-tumor role.
In this case, targeting the macrophages and improving their impact draws in T cells and the adaptive immune response.
Interestingly, Kim and colleagues found most macrophages summoned to the tumors by the combination were bone marrow-derived monocytes rather than microglia, the antigen-presenting cells most active in the central nervous system.
For a complete list of co-authors, please see the paper.
This research was supported by grants from the National Institute of Neurological Disorders and Stroke (RO1 NS104315), the Cancer Prevention & Research Institute of Texas, the American Brain Tumor Association, the National Cancer Institute (KO8 CA21070) and the Preston A. Wells, Jr. Endowment at the University of Florida.
This combination therapy is ready for clinical trials.
Betty Y.S. Kim, M.D., Ph.D.
Physician & Researcher
