MD Anderson Research Highlights for June 27, 2023
Featuring end-of-life treatment disparities, novel treatment targets to improve immunotherapy responses, and strategies to manage immune-related toxicities
MD Anderson News Release June 27, 2023
The University of Texas MD Anderson Cancer Center’s Research Highlights showcases the latest breakthroughs in cancer care, research and prevention. These advances are made possible through seamless collaboration between MD Anderson’s world-leading clinicians and scientists, bringing discoveries from the lab to the clinic and back.
Recent developments include the identification of disparities in end-of-life immunotherapy treatment, a new target to improve immunotherapy responses in KRAS-mutant lung cancer, a new connection for small RNAs in anti-tumor immunity and obesity, the benefits of fecal microbiome transplants in improving immune-mediated colitis, and insights into the use of IL-6R therapy to treat immune-related toxicities.
Race, insurance and practice setting associated with use of immunotherapy in end-of-life systemic treatment
Black patients or those with Medicaid were less likely to receive immunotherapy during end-of-life cancer treatment compared to white patients and those with commercial insurance, according to a new study led by Kerin Adelson, M.D., and colleagues. In addition, treatment at community practices was associated with a higher likelihood of receiving 30-day systemic end-of-life treatment compared to treatment at academic centers. Researchers investigated factors that contributed to the use of antineoplastic end-of-life systemic treatment and evaluated the real-world electronic health record-derived and de-identified database of 53,791 adult patients with advanced or metastatic solid tumor cancers. To ensure quality care for patients, further examination of the contributing factors is warranted in order to understand the impact on downstream acute care use, hospice transition, quality of life and cost. Learn more in the Journal of Clinical Oncology.
Targeting lactate secretion may reverse immunotherapy resistance in patients with LKB1-deficient lung cancer
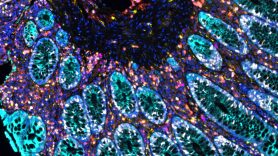
Scientists have discovered that blocking lactate secretions can enhance the effectiveness of immunotherapy in patients with KRAS-mutated lung cancer. Led by John Heymach M.D, Ph.D., the study reveals a lack of the protein LKB1, which plays a crucial role in immune response against tumors, produces elevated levels of lactate. The lactate negatively affects the immune response by attracting suppressive immune cells (M2 macrophages) and impairing the function of T cells. The research demonstrates blocking either the lactate transporter protein, MCT4, in tumor cells or the lactate receptor on immune cells can reverse the detrimental effects caused by the lactate and restore the anti-tumor immune response. These findings were observed in both mouse models and tumors from patients with STK11 gene mutations. While further research is necessary to validate these findings in humans, the data provides a possible strategy in reversing immunotherapy resistance in mutant lung cancer. Learn more in Cancer Cell.
Small nucleolar RNA linked to obesity and impaired NK anti-tumor immunity
Obesity is associated with an increased risk of cancer metastasis and treatment resistance, but the underlying mechanisms are not well known. Interleukin-15 (IL-15) is a known stimulator of immune cells, and studies suggest that plasma IL-15 levels are negatively correlated with body mass index (BMI). Additionally, small nucleolar RNAs (snoRNAs) recently have been implicated as biomarkers for a variety of cancers. This guided researchers led by Chunru Lin, M.D., Ph.D., and Liuqing Yang, Ph.D., to profile snoRNAs in serum from obese human donors, discovering that SNORD46 was overexpressed and correlated with IL-15 and BMI. Lab models that overexpressed SNORD46 developed obesity and had impaired anti-tumor immunity, caused by the inhibition of the IL-15 pathway in natural killer (NK) cells. Using a snoRNA power inhibitor to block SNORD46 resulted in anti-obesity effects and improved anti-tumor immunity of chimeric antigen receptor (CAR) NK cell therapy. These findings highlight the importance of snoRNAs in obesity and in the immune response, demonstrating their therapeutic potential. Learn more in Cell Metabolism.
Fecal microbiota transplants effective for refractory immune-mediated colitis
Immune checkpoint inhibitors are effective for many patients with cancer, but they can increase the risk of mild to severe immune-mediated colitis (IMC), emphasizing a need to identify additional therapies to avoid care disruption. Previous studies suggest fecal microbiota transplantation (FMT), which delivers healthy human donor stool to a recipient, can help restore the gut microbiome balance and improve treatment responses. In the largest case series to date, researchers led by Yinghong Wang, M.D., Ph.D., and Robert Jenq, M.D., evaluated FMT in 12 patients with refractory IMC who failed to respond to standard first-line corticosteroids and second-line treatments. Ten patients (83%) achieved symptom improvement and 92% achieved IMC clinical remission. The researchers noted significant increases in specific bacterial signatures that may play a role in improving the immune response. This study demonstrated the promise of FMT as a therapeutic strategy to better manage toxicities associated with checkpoint blockade. Learn more in Science Translational Medicine.
Targeting IL-6R may improve immune-related toxicities without blunting anti-tumor immunity
Immunotherapy can significantly improve outcomes for many patients, but immune-related toxicities remain a major challenge. While therapies targeting the interleukin-6 receptor (IL-6R) can improve immune-related adverse events (irAEs), its impact on anti-tumor immunity are unknown. Therefore, researchers led by Adi Diab, M.D., and Noha Abdel-Wahab, M.D., Ph.D., performed a retrospective analysis of 92 patients who received anti-IL-6R treatment for corticosteroid-refractory irAEs or flare of pre-existing autoimmune disease following checkpoint blockade. The study found 73% of patients showed improvement of irAE after anti-IL-6R therapy, while 7% of patients discontinued IL-6R therapy due to adverse events. Of 70 patients that could be evaluated for tumor response, the overall response rate (ORR) was identical before and after anti-IL-6R therapy, suggesting it did not hinder anti-tumor immunity. The results suggest further evaluation of the safety and efficacy of this treatment in combination with checkpoint blockade is warranted. Learn more in the Journal for ImmunoTherapy of Cancer.
In case you missed it
Read below to catch up on recent MD Anderson press releases.
- New understanding of why kidney cancers become metastatic discovered by MD Anderson researchers
- MD Anderson and Ochsner Health announce partnership to create first fully integrated cancer program in Louisiana
- Mutant KRAS regulates Y chromosome gene in colorectal cancer, driving metastasis and inhibiting anti-tumor immunity
- MD Anderson and Replay announce FDA clearance of IND application for first-in-class TCR NK cell therapy for sarcoma
- Adagrasib effective for patients with KRAS G12C-mutant lung cancer and untreated brain metastases
- Patients with refractory metastatic colorectal cancer experience survival benefits with fruquintinib
- Study brings new understanding of multiple myeloma evolution