Podcast: Advancing pancreatic cancer research
request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Pancreatic Cancer
- Pancreatic Cancer Research
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsPancreatic Cancer Research
As one of the world's largest and most experienced comprehensive cancer centers, MD Anderson’s research experts are leading the effort to better treat pancreatic cancer, as well as design more sensitive screening procedures to detect this disease at earlier stages. Our patients benefit from the most advanced pancreatic cancer research, translated into clinical practice as quickly as possible.
Due to the location of the pancreas, detection of tumors at a time early enough to be eligible for surgical removal is rare. Our researchers are working to change that by creating a blood test that signals the presence of cancer. Researchers from across the intitution are focusing on subsets of patients that are at high risk for pancreatic cancer, including those with pancreatic “cysts” or new-onset diabetes above the age of 50 years. When developed, this highly sensitive and specific test will detect abnormal molecules that are shed from tumors before the appearance of pancreatic cancer symptoms.
To complement this strategy, we’re also investigating new imaging techniques to visualize pre-cancerous pancreatic lesions called PanINs (pancreatic intraepithelial neoplasias) to detect early precursors of pancreatic cancer. The long term goal of these efforts is to improve the survival rate of pancreatic cancer patients by intercepting pancreatic cancer before it becomes deadly.
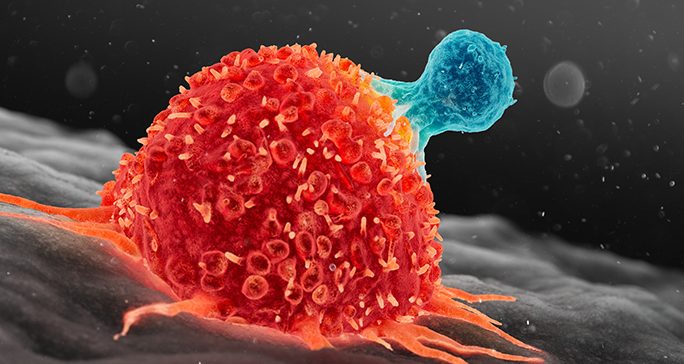
We’re also investigating new treatment options for patients with pancreatic cancer. Through preclinical studies, our researchers have identified a tumor-promoting pathway that, when inhibited, reduces the rate of resistance to validated targeted therapy drugs. We’re developing a drug targeting this pathway that will soon enter Phase I trials. We’re also exploring ways to use new and personalized immunotherapy approaches to enhance a patient’s own immune cells to better fight their pancreatic cancer.
Through our cutting-edge pancreatic cancer research, MD Anderson has:
- Initiated the first pancreatic cancer high-risk clinic, where family members and those at higher risk for pancreatic cancer (such as adults with new onset diabetes) can be screened and advised.
- Pioneered the advance of using chemotherapy before surgery (so-called “neoadjuvant therapy”) to enhance the effectiveness of pancreatic tumor resection. Patients who complete their neoadjuvant therapy and successfully undergo surgery have, on average, significantly longer survival than those who receive upfront surgery.
- Developed a long-term, personalized program to monitor pancreatic cancer patients using serial blood draws (“liquid biopsies”). This program allows us to map their tumor’s response to therapies and predict recurrent disease before it appears

Pancreatic Cancer Research Stories
Clinical Trials
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.