Rezvani Lab
Katy Rezvani, M.D., Ph.D
Professor, Stem Cell Transplantation and Cellular Therapy
Principal Investigator
- Departments, Labs and Institutes
- Labs
- Rezvani Laboratory
Areas of Research
- Immunotherapy
- Immunology
- Genetics
- CAR T-cells
- CAR NK-cells
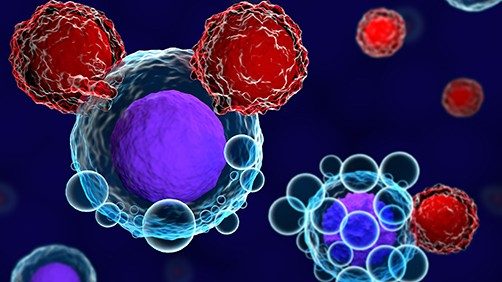
The Rezvani laboratory broadly focuses on the role of natural killer (NK) cells in mediating protection against hematologic malignancies and solid tumors and strategies to enhance killing function against various cancer.
Current Discovery and Research Themes in the Rezvani Laboratory
- Comprehensive analysis of NK cells and their receptors in cancer following hematopoietic stem cell transplantation using mass cytometry (CyTOF) and transcriptomic profiling.
- Engineering NK cells to express chimeric antigen receptor (CAR) and cytokine genes to enhance their effector function and persistence.
- Understanding mechanisms of NK immune evasion and using gene editing tools to target checkpoints to enhance NK effector function.
- Enhancing T cell function against viruses and cancer antigens using CARs and gene editing tools such as CRISPR.

Click to enlarge photo
Open Positions
Postdoctoral positions are currently available in the Rezvani Lab. Inquiries should be sent to Katy Rezvani, M.D., Ph.D.
Contact the Lab
Katy Rezvani, M.D., Ph.D.
Principal Investigator
Professor, Stem Cell Transplantation & Cellular Therapy department
KRezvani@mdanderson.org
Cancer patients with rare deadly brain infection treated...
An emerging treatment known as adoptive T-cell therapy has proven effective in a Phase II clinical trial for treating progressive...
Give Now
Your gift will help make a tremendous difference.
Research Areas
Find out about the four types of research taking place at MD Anderson.
Subscribe
Get the latest information on our cancer breakthroughs.