Hold On - Gregory Lizee, Ph.D.
News and Media
Novel immunotherapy delivery approach safe and beneficial...
A novel approach to administer intrathecal (IT) immunotherapy (directly into the spinal fluid) and intravenous (IV) immunotherapy was...
Neoadjuvant immunotherapy with relatlimab and nivolumab is...
Giving the combination of immune checkpoint inhibitors relatlimab and nivolumab to patients with stage III melanoma before surgery was...
Targeting interleukin-6 could help relieve immunotherapy...
Researchers at The University of Texas MD Anderson Cancer Center have identified a novel strategy to reduce immune-related adverse...
MD Anderson receives nearly $19.4 million in CPRIT funding
The University of Texas MD Anderson Cancer Center today was awarded 15 grants totaling $19.38 million from the Cancer Prevention and...
High-fiber diet associated with improved progression-free...
Patients with melanoma who reported eating more fiber-rich foods when they began immunotherapy treatment survived longer without...
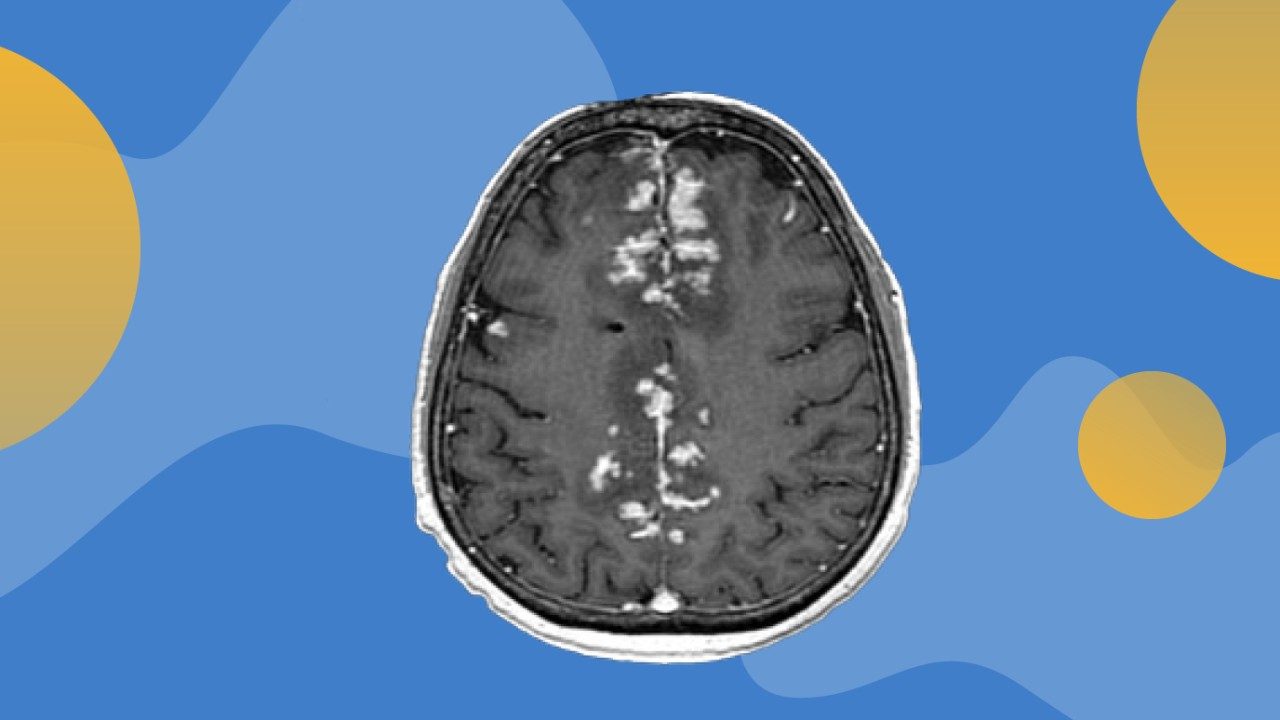
Metastatic melanoma survivor grateful for immunotherapy...
Last updated March 18, 2022.
When Bob Seibert reflects on the nearly one and half years since his stage IV melanoma diagnosis, there...

Hold On by Gregory Lizee, Ph.D.
Hold On, was written by Greg Lizee, a researcher in the Melanoma Medical Oncology Department.
Give Now
Your gift will help make a tremendous difference.
Research Areas
Find out about the four types of research taking place at MD Anderson.
Subscribe
Get the latest information on our cancer breakthroughs.