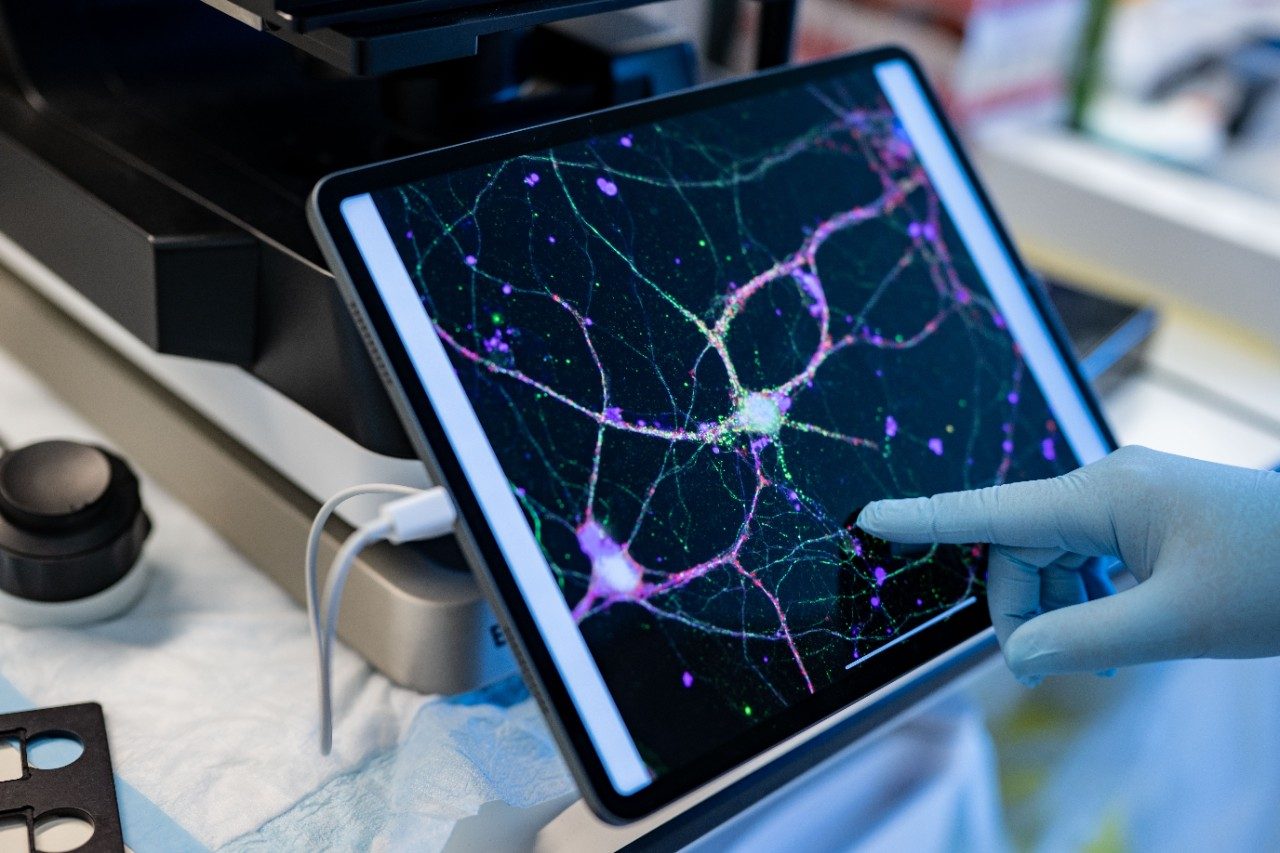
Using math to answer cancer’s biggest questions
One of the most important parts of science is asking the right questions. As an engineer trying to break into medical research, Joseph Butner, Ph.D., found that some of the questions he was trying to answer weren’t actually all that important to oncologists in the clinic and they weren’t translating into new or better treatments for patients.
But Butner was certain that if the right mathematical methods that have traditionally been used to solve engineering and physics problems were applied to medicine, then he could tap into opportunities and advancements in therapeutic approaches that could change patients’ lives.
Tips for using AI to find cancer information
Can breastfeeding really lower your breast cancer risk?
Should you be getting regular mental health checkups?
Astrocytoma survivor gives back to MD Anderson
10 thyroid myths you shouldn’t believe
|
Diagnosis & Treatment
|
|---|
|
Healthy Living
|
|
Diagnosis & Treatment
|
|
Diagnosis & Treatment
|
|
Diagnosis & Treatment
|
Find stories by topic
Find out everything you need to know to navigate a cancer diagnosis and treatment from MD Anderson’s experts.
Should you be getting regular mental health checkups?
July 07, 2025
10 thyroid myths you shouldn’t believe
July 02, 2025
Vasectomy and prostate cancer risk: What you should know
June 26, 2025
5 little-known breast cancer facts
June 24, 2025
Preventing and managing caregiver burnout
June 23, 2025
Anoscopy explained: Purpose, process and results
June 19, 2025
Read inspiring stories from patients and caregivers – and get their advice to help you or a loved one through cancer.
Astrocytoma survivor gives back to MD Anderson
July 03, 2025
Lymphoma survivor uses AI to help explain her treatment
June 20, 2025
Get MD Anderson experts’ advice to help you stay healthy and reduce your risk of diseases like cancer.
Can breastfeeding really lower your breast cancer risk?
July 08, 2025
Is BMI the best body weight calculator?
July 01, 2025
5 little-known breast cancer facts
June 24, 2025
What should you look for in a sun hat?
June 19, 2025
6 ways to cope with scanxiety
June 17, 2025
Do weighted vests benefit your fitness routine?
June 16, 2025
Seeds: The ‘unsung hero’ of plant-based nutrition
June 13, 2025
Learn how MD Anderson researchers are advancing our understanding and treatment of cancer – and get to know the scientists behind this research.
Using math to answer cancer’s biggest questions
July 09, 2025
What causes chemobrain? New insights
June 03, 2025
Nutrivention: Food as medicine
May 28, 2025
5 emerging therapies presented at ASCO 2025
May 28, 2025
Top 5 MD Anderson abstracts at AACR 2025
April 25, 2025
Cell therapy: The evolution of the ‘living drug’
April 22, 2025
How non-scientists are helping cancer researchers
February 21, 2025
Read insights on the latest news and trending topics from MD Anderson experts, and see what drives us to end cancer.
Tips for using AI to find cancer information
July 10, 2025
What is a Living Will?
June 06, 2025
Surgeon-scientist: ‘MD Anderson is unique’
May 15, 2025
Find out what inspires our donors to give to MD Anderson, and learn how their generous support advances our mission to end cancer.
Mom's legacy lives on through fundraising for MD Anderson
April 28, 2025
Three cancer survivors raise funds to support Colorado patients
October 03, 2024
Inflammatory breast cancer survivor finds hope at MD Anderson
October 24, 2023