Utilizing the body’s natural born killers
Unique access to cord blood gives MD Anderson cancer experts a big advantage in harnessing and using these immune cells against the disease

Daniel Esqueda, senior clinical cell therapy specialist, retrieves frozen cord blood to be thawed for natural killer cell production when a patient is scheduled for treatment.
photo by Nick de la Torre
Natural killer cells sound menacing, but they play a friendly role in keeping us healthy. And they might do much more in stopping cancer.
After years of diligent, groundbreaking research, MD Anderson physician-scientists are putting natural killer cells – NK cells for short – to work in a series of clinical trials for a variety of cancers through the cancer center’s Moon Shots Program™.
“These white blood cells are the scouts, the sentinels of our immune system,” says Elizabeth Shpall, M.D., professor of Stem Cell Transplantation and Cellular Therapy.
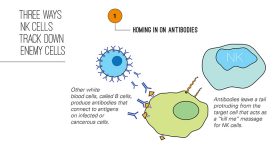
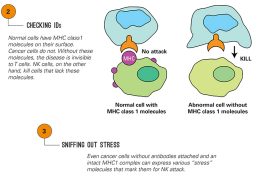
They’re constantly surveying our bodies for invading microbes and abnormal cells – the type that can become cancer if they aren’t already. Equipped with an array of detection techniques, natural killers also are heavily armed to deal with the threats they discover.
“They’re poised to kill. They can kill over and over again,” says Katy Rezvani, M.D., who is also a professor in the department. “That’s why we’re trying to harness them for cancer immunotherapy.”
To do that, Shpall, Rezvani and their colleagues have been systematically identifying and overcoming disadvantages that hinder NK cells as cancer-fighting tools.
High on the list: There aren’t enough of them – they make up only 10% to 15% of our blood cells – and they don’t persist, lasting only two to three weeks. And perhaps most importantly, by the time a patient’s cancer has matured, it’s already evolved ways to evade that patient’s NK cells, so cells from a donor are required.

Enter umbilical cords
To get donor cells, Shpall and her colleagues have tapped a resource that’s unique for a cancer center, an umbilical-cord blood bank. MD Anderson’s was established as a source of blood stem cells for patients with certain blood cancers. Today, the bank stores 27,000 units of cord blood cells donated by mothers from Houston-area hospitals.
This resource means there’s no need to search for donors willing to go through safety screening and cell collection. Another advantage:
The cord blood units have been thoroughly analyzed, so it’s simple to select a good match with high potential for expanding in the lab.
To increase the supply of cord blood NK cells, Shpall’s team applies a technique pioneered by researchers in MD Anderson’s Pediatrics department nearly a decade ago for patients needing their own supply of stem cells expanded. The technique makes it possible to isolate and stimulate the NK cells in the lab, increasing their numbers 200-to 500-fold.
These NK cells can be given to patients without fear of dangerous side effects like graft vs. host disease. NK cells have been given to hundreds of patients, and so far there have been no toxicities.
“With the cord blood bank, we can have off-the-shelf products, NK cells that can be given to patients without a need to individualize them,” Rezvani says.
Having overcome two major barriers – the need for donor cells and lots of them – the team now is working on ways to genetically modify NK cells so they last longer, even though cord-blood-derived NK cells provide some improvement in lifespan.
And the team is looking to add specialized receptors to identify and destroy specific targets.
“Some tumor types are more resistant to NK cells than others, and our preclinical models show that adding one of these receptors to NK cells makes those cancers more sensitive to NK cells,” Rezvani says.

Clinical trials underway
Five clinical trials at MD Anderson deploy NK cells against Hodgkin and non-Hodgkin lymphoma, several types of leukemia, myelodysplastic syndrome and multiple myeloma.
Three of the trials administer NK cells from cord blood in conjunction with transplants using blood stem cells from donors.
“NK cells are the first cells to recover after a blood stem cell transplant, and many studies show NK activity prevents disease relapse,” Rezvani says. So adding cord blood NK cells is a logical attempt to strengthen transplants.
A fourth trial, for multiple myeloma, combines an infusion of cord blood NK cells with an autologous transplant, in which a patient’s own blood is used.
“Autologous stem cell transplants can result in prolonged remission for some patients, but they aren’t curative,” Shpall says. “If we add cord blood NK cells to the stem cell transplant, maybe we can break that barrier. The same applies to our acute myeloid leukemia studies.”
Early results in the multiple myeloma trial showed that NK cells took hold and were well tolerated by patients; however, the impact on remission and survival remains to be seen.
The fifth trial combines NK cells with chemotherapy and an immunealtering drug called lenolidamide in a variety of blood cancers.
Rezvani and Shpall expect NK cells to be deployed against solid tumors as well, with the first trial planned against glioblastoma multiforme, the most common and deadliest of brain tumors.
To further extend the reach of this approach, MD Anderson has signed agreements with three pharmaceutical companies to test its NK cells in combination with the companies’ own experimental therapies.
NK cells remain in the early stages of development as a cancer treatment.
While others also are studying these cells, MD Anderson has unique advantages.
Moon shots and NK cells
Shpall is co-leader of the Adoptive Cell Therapy Platform™ of MD Anderson’s Moon Shots Program™ to reduce cancer deaths by accelerating development of therapies from scientific discoveries.
The platform provides NK cell and T cell therapies to the individual Moon Shots. Those currently using NK cells in clinical trials and those that have studies planned include:
- Acute Myeloid Leukemia/Myelodysplastic Syndrome Moon Shot
- High-Risk Multiple Myeloma Moon Shot
- Chronic Lymphocytic Leukemia Moon Shot
- B Cell Lymphoma Moon Shot
- Glioblastoma Moon Shot












