Degrees of separation: Science stars are born at graduate school
Wilderness doctor Matt Lewin, M.D., Ph.D., has traveled to the ends of the Earth treating scientists who work in remote and dangerous locations.
As an expedition doctor with the California Academy of Sciences, he’s handled dehydration in the Gobi Desert, poisonous spider bites in Papua, New Guinea, and altitude sickness in Argentina.
But one of the biggest challenges, Lewin says, is saving victims of venomous snakebites, which he deems “the world’s most neglected tropical disease.”
Neglected, he says, because 75% of snakebite victims who die never make it to a hospital.
“When you’re deep in a rainforest or high atop a mountain on a scientific expedition, medical treatment can be hours or even days away,” Lewin explains.
When a venomous snake bites, it can send paralyzing neurotoxins coursing through the victim’s veins. The nervous system becomes progressively disabled, and death comes when neurotransmission ceases. With no instructions to breathe, the muscles of the diaphragm are stilled and the victim asphyxiates.
Hospitalization can provide anti-venom and respiratory support to counter these effects, but in the most remote regions of the globe, there often is no anti-venom, no respirator and, sometimes, no way out.
To protect scientists on future expeditions, Lewin invented a portable, field-friendly nasal spray that contains an antidote to some snake venoms that cause paralysis. Typically, anti-venom is administered through an intravenous (IV) injection, but Lewin thinks clinical trials will prove the nasal spray to be quicker, cheaper and likely equally as effective.
“It’s easy to administer in the field,” he says, “because no needles are required. And unlike IV anti-venom, it doesn’t have to be refrigerated.”
Lewin tested the treatment on himself in an experiment that took place at the University of California San Francisco Medical Center. Surrounded by several anesthesiologists and an emergency room doctor, he was paralyzed while still awake with a toxin that mimics cobra venom. The team then administered the nasal spray, and within 15 minutes Lewin completely recovered, though the paralyzing toxin was still being delivered into his bloodstream.
In India, where an estimated 1 million people are bitten by snakes every year, the nasal spray was successfully used to treat a patient who did not respond to anti-venom therapy. The spray has also been successfully tested in laboratory mice that were injected with high doses of cobra venom. Clinical trials are in the works, and when made widely available, the spray is expected to save tens of thousands of lives each year.
Shaping scientists
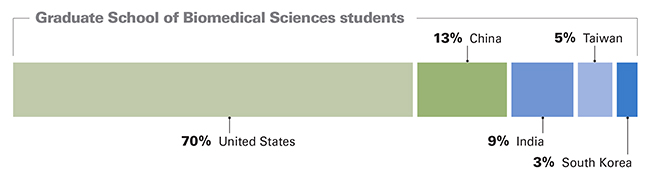
As a student, Lewin honed his science skills at the University of Texas Graduate School of Biomedical Sciences, where he graduated in 1999. Nestled in the heart of the Texas Medical Center and located in MD Anderson’s George and Cynthia Mitchell Basic Sciences Research Building, the school offers graduate-level degrees to students preparing for careers as bio-medical scientists. Master’s and doctorate degrees are available in fields such as cancer biology, experimental therapeutics, immunology, human and molecular genetics, and clinical and translational sciences. Students can earn a Ph.D., M.S. or, like Lewin, a combination M.D./Ph.D. degree.
“We’re training the next generation of scientists passionate about tackling problems in human diseases through laboratory research conducted at the cellular and molecular levels,” says Michelle Barton, Ph.D., one of the school’s two deans.
In a unique collaboration, the school is run by two institutions — MD Anderson and The University of Texas Health Science Center at Houston. Faculty and deans (Barton and Michael Blackburn, Ph.D.) come from both institutions.
Since its founding in 1963, the school has produced a steady stream of science “superstars” who make important discoveries that advance cancer care and knowledge of other diseases and conditions.
Matt Lewin, M.D., Ph.D., ’99

“I still lean heavily on what I learned at the Graduate School of Biomedical Sciences. The environment was, and continues to be, fabulously supportive. I graduated 15 years ago, and I still consult my mentors there about scientific matters.”
Suzanne Fuqua, Ph.D., ’82

Fuqua answered a question that puzzled scientists for years when she discovered why the drug tamoxifen stops working in some breast cancer patients. Certain breast cancers use the hormone estrogen as “fuel.” The more estrogen the cancerous tumors are exposed to, the more they grow and spread. Tamoxifen works by blocking estrogen, thereby depriving tumors of their “fuel.” Unfortunately, tamoxifen’s anti-tumor effect dwindles in about half of patients treated with the drug. Fuqua, who is a professor in Baylor College of Medicine’s Lester and Sue Smith Breast Center, discovered that women who have inadequate levels of a protein known as Rho GDI are more likely to resist tamoxifen and similar drugs, which can allow cancer to spread. This discovery is being used to develop new drugs that stop new tumors from forming.
John Kopchick, Ph.D., ’80

Kopchick specializes in human growth hormone research. His discoveries led to the development of a drug named Somavert, which treats acromegaly, a form of gigantism. In this condition, the body makes too much human growth hormone (HGH), which causes organs and bones to grow overly large. If not treated, acromegaly can cause disfiguration or death. Lately, as a distinguished professor of molecular biology at Ohio University, Kopchick has been working to find a biomarker that can be used to detect illegal use of HGH in athletes. Because HGH is virtually undetectable, it is thought to be the “drug of choice” among athletes who take performance-enhancing substances.
“My experience at the graduate school was second to none. As a graduate student, I learned how to form and test hypotheses, how to design and carry out experiments, and how to interpret results. My colleagues and I published our work and presented it at national and international meetings. We worked hard, but we played hard, too. Our lab group was like a ‘family,’ often spending long hours together in the lab and socializing together on weekends. We still stay in touch.”
— John Kopchick, Ph.D.
Hugo Barrera-Saldana, Ph.D., ’82

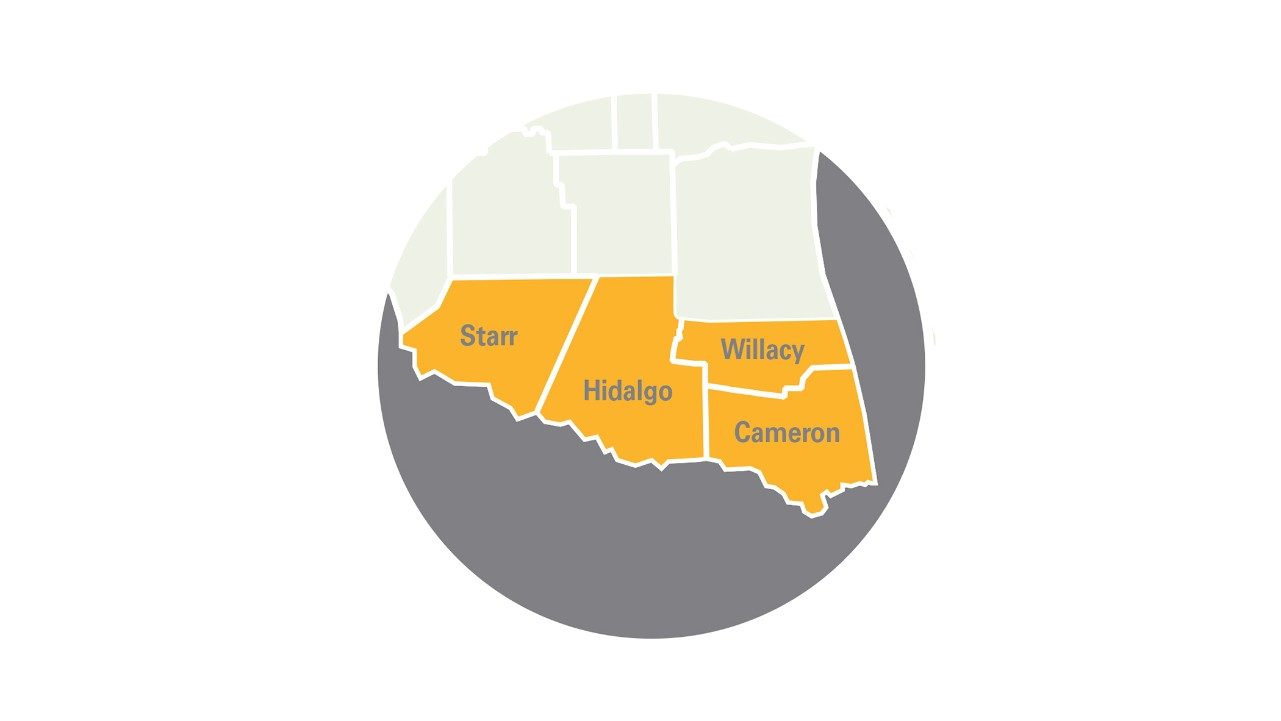
Barrera-Saldana learned first-world science in the U.S. and Europe, then took what he learned back to his native Mexico, where scientists often struggle for recognition and funding. After completing his undergraduate education at the Autonomous University of Nuevo Leon in Mexico, Barrera-Saldana made his way to Texas and became the first student from that country to enroll at the GSBS. After earning a Ph.D., conducting postdoctoral research in Europe and publishing a string of scientific papers, Barrera-Saldana was primed for a successful science career in the U.S. Instead, he headed back to Mexico to offer the next generation of students the benefit of his science education. Today, he’s a professor of Biochemistry and Molecular Medicine, head of the Genomic Science Laboratory, and secretary of science and technology at the Autonomous University of Nuevo Leon’s Medical School. He founded a medical biotech company and is helping modernize human genetics research centers throughout Mexico, Colombia, Venezuela and Peru.
Danny Welch, Ph.D., ’84

Welch discovered six of the 30 known metastasis suppressors — proteins that act to slow or prevent the spread of cancer. Work is underway to translate his discoveries into drugs that “hold” cancer cells in a dormant state. Instead of requiring total elimination of all cancer cells for a cure, these suppressor drugs could make metastatic cancer a chronic, controllable disease. As Welch explains it, “it may not be necessary to corral the horse in the stable as long as it can be kept from running amok beyond the pasture.” Welch is a professor and chair of the Department of Cancer Biology at the University of Kansas Medical Center.
“The esprit de corps at the graduate school was as much a part of my scientific and personal growth as the formal training. The Friday beer busts were a great chance to interact with everyone, including the dean. There was never any pretense. Rather, there was a sense of camaraderie. I knew my fellow students and faculty had my back if I ever wanted to try something scientifically risky. They’ve still got my back, and I theirs.”
— Danny Welch, Ph.D.