Engineering, cancer biology form attraction

Ang at radiation oncology forefront for head, neck
By Laura Sussman
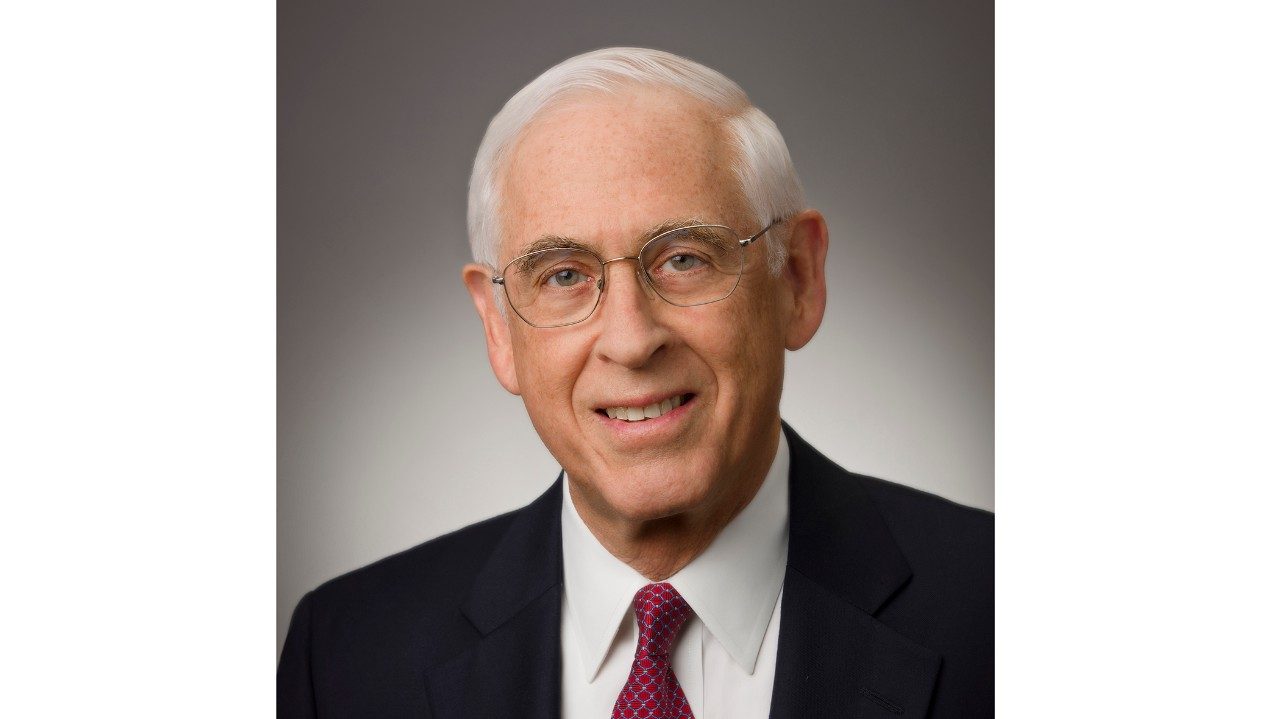
Kie-Kian Ang’s interest in engineering attracted him to radiation oncology. But it was the disease’s biology that drew him to his specialty, head and neck cancers.
With more than 25 years experience at MD Anderson, Ang, an M.D., Ph.D., is at the forefront of the field’s modern milestones, including the discovery of how to sensitize head and neck cancers to radiation and the improvement of radiation technologies, such as intensity modulated radiation therapy and proton therapy.
Recently, an analysis of an international Phase III clinical trial led by Ang — the largest, most definitive study to date — found that a strong and independent prognostic factor for survival in head and neck cancer patients is the presence of the human papilloma virus.
When researchers adjusted for other significant determinants of survival, oropharyngeal cancer patients with advanced HPV-positive cancer had a 58% reduction in risk of death, compared to patients with HPV-negative tumors.
Excellent prognosis
“This is the strongest factor we’ve identified for head and neck cancer,” says Ang, professor in the Department of Radiation Oncology. “Its value is stronger than any other prognostic factors, such as size of tumor or lymph node involvement. Knowing that the tumor is associated with HPV is telling patients that their prognosis is excellent with currently available treatments.”
Reported in June at the 2010 annual meeting of the American Society of Clinical Oncology.
Although MD Anderson focuses on cancers of the head and neck, it was rated No. 6 among all types of ear, nose and throat programs in the nation in the U.S. News & World Report’s 2010 “Best Hospitals” survey.
Multiple steps lead to improved emergency care
By Julie Penne
In the past few years, MD Anderson’s growing and changing patient population led the Emergency Center to take on characteristics of a general hospital with overcrowding, long waits and stretched staff.
Changing these traits has taken a task force and ongoing efforts to meet these challenges and those of increasingly sophisticated clinical trials and complex patients.
A year after the task force went to work, MD Anderson’s vital 24/7 unit not only sees more and sicker patients than ever, but they are also treated faster with better outcomes.
More than 1,700 patients are seen monthly, and the percentage of severely ill has increased from about 4% to 7%. Wait times have decreased from about 15 hours to eight hours.
Quite a turnaround
“To turn around the Emergency Center and deliver the best care possible in the most efficient manner, we needed to better align our clinical and staff resources, transition care more effectively, streamline work flow and processes, integrate information technology and renew the motivation of the faculty and staff who care for our critically ill patients,” says Paul Mansfield, M.D., professor in the Department of Surgical Oncology and head of Emergency Services.
A new academic Department of Emergency Medicine also was established to prepare physicians and other health care professionals for this critical discipline, and seize research and education opportunities to improve how emergency care is rendered.
Brady helps patients take control of their diabetes
By Mary Brolley
There are many ways to greet a medical professional at that first appointment.
Veronica Brady has heard a few. “One patient’s first words were, ‘Are you as mean as you look?’” she recalls. “I looked right back at him and said, ‘Every bit.’”
An advanced practice nurse in the Diabetes Program in the Department of Endocrine Neoplasia and Hormonal Disorders, Brady rarely encounters resistance from patients. In fact, many are eager to take control of this aspect of their health, she says.
Patients referred to the program receive education about diabetes and glucose monitoring, counseling on diet and exercise, and a dose of reassurance that diabetes can be managed.
Nursing background helps
Brady is uniquely suited to this calling, having worked as an oncology nurse for more than a dozen years before switching into diabetes care. She was one of the first nurse practitioners recruited into the four-year-old program, which is attracting increased notice nationally.
And the patient who thought she looked mean? Brady laughs. “At the end of the appointment, he said, ‘You know what? I’m in your hands.’”
Although MD Anderson’s Department of Endocrine Neoplasia and Hormonal Disorders is dedicated solely to treatment of cancer patients, it rose in ratings to No. 21 in the nation among all hospitals treating endocrine disorders in U.S. News & World Report’s 2010 “Best Hospitals” survey.