- Treatment Options
- Ablation Therapy
- Angiogenesis Inhibitors
- Awake Craniotomy
- Brachytherapy
- Breast Reconstruction Surgery
- CAR T Cell Therapy
- Chemotherapy
- Cryoablation
- High-Intensity Focused Ultrasound (HIFU)
- Histotripsy
- Hyperthermic Intraperitoneal Chemotherapy
- Immunotherapy
- Immune Checkpoint Inhibitors
- Integrative Medicine
- Interventional Oncology
- Laser Interstitial Thermal Therapy (LITT)
- Microwave Ablation
- Minimally Invasive Surgery
- MR-Linac Radiation Therapy
- Palliative Care
- Proton Therapy
- Radiation Therapy
- Radiofrequency Ablation
- Stem Cell (Bone Marrow) Transplantation
- Stereotactic Body Radiation Therapy
- Stereotactic Radiosurgery
- Surgery
- Targeted Therapy
- Y90 Radioembolization
Immunotherapy
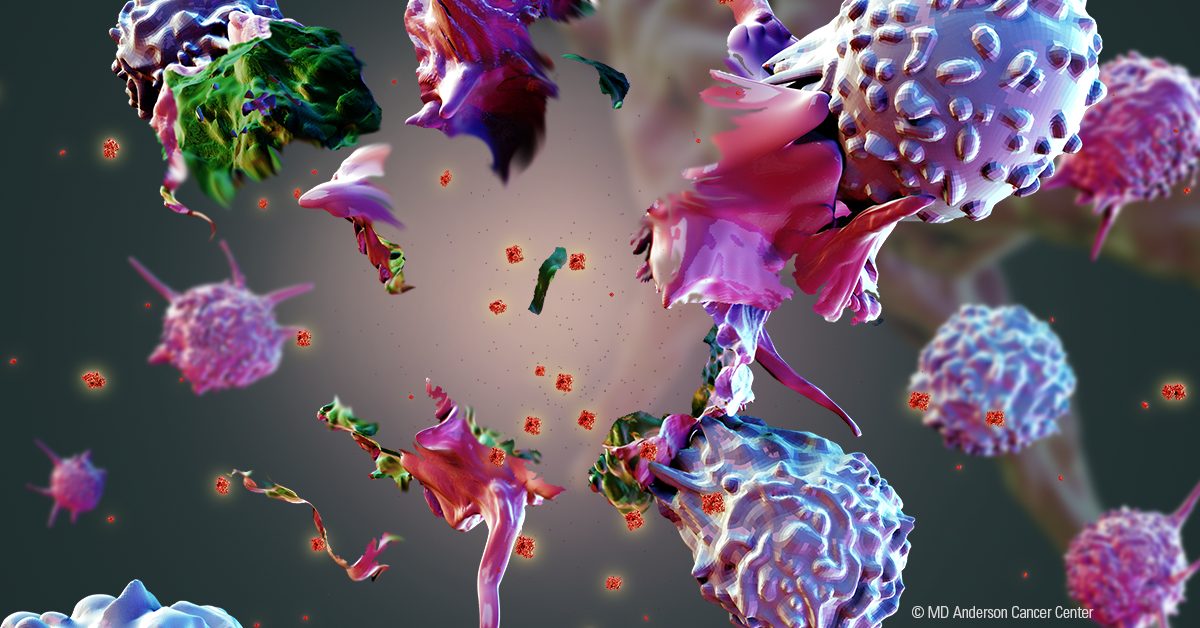
Immunotherapy is a treatment that uses a person's immune system to eliminate cancer.
The immune system finds and defends the body from infection and disease. Cancer is a complex disease that can evade and outsmart the immune system. It’s often not recognized until it has already become too difficult to handle. Immunotherapy can improve the way an immune system works, allowing it to find and get rid of cancer cells.
There are several types of immunotherapies, and each helps the immune system in a different way.
Types of immunotherapy
Immune checkpoint therapy helps cancer-fighting immune cells, called T cells, mount a longer-lasting response against the cancer.
Adoptive cellular therapy increases the number and/or effectiveness of immune cells, usually T cells, which improves the power of the immune response against the cancer. There are four main types of adoptive cellular therapy:
- Chimeric antigen receptor (CAR) T cell therapy gives patients large amounts of T cells that are all genetically engineered to find and fight the cancer.
- Chimeric antigen receptor (CAR) natural killer (NK) cell therapy is a promising new cellular immunotherapy that is still in clinical trials. NK cells are immune system cells that identify and then kill abnormal cells, including some cancer cells. Many cancers are good at avoiding detection, though. This limits the ability of NK cells to fight the disease naturally. In CAR NK cell therapy, NK cells are engineered to better recognize cancer, boosting their ability to find and kill cancer cells. Researchers do this by collecting NK cells from donated umbilical cord blood. They then add a molecule known as a chimeric antigen receptor, or CAR, to the NK cells. This CAR recognizes a molecule on the surface of cancer cells, enabling the CAR NK cells to better find and fight cancer.
- Tumor infiltrating lymphocyte (TIL) therapy uses a patient’s T cells that are collected from a piece of surgically-removed tumor. While these cells may recognize the cancer, there are too few of them to succeed. The number of these cells is increased substantially in the lab and then given back to the patient.
- Endogenous T cell (ETC) therapy uses T cells from a patient’s blood. From this diverse pool of T cells, doctors select only those that may recognize signatures specific to the cancer. The number of these specific T cells is increased substantially and then given back to the patient.
Cancer vaccines help the body recognize cancer cells and stimulate the immune system to destroy them. Cancer vaccines usually contain one of the following:
- cancer cells taken from the patient’s tumor
- proteins designed to attach themselves to cancer cells
- proteins specific to a patient’s tumor
Monoclonal antibodies attach to specific proteins on the surface of cancer cells or immune cells. They either:
- mark the cancer as a target for the immune system, or
- boost the ability of immune cells to fight the cancer
Cytokine therapy relies on proteins called interferons and interleukins to trigger an immune response. Interleukin-2 (IL-2) is used to treat kidney cancers and melanomas that have spread to other regions of the body. Interferon alpha (IFN-alpha) is currently being used to treat melanoma, kidney cancer and certain leukemias and lymphomas. These cytokine treatments are also being combined with other types of immunotherapies to increase their effectiveness.
Each type of immunotherapy has distinct side effects. Moreover, certain immunotherapies are more effective for some types of cancer than others. A patient’s overall health and type of cancer determines which immunotherapies are available to them.
Sometimes two different types of immunotherapies are combined during treatment. Other times, a single immunotherapy is used with another type of therapy, such as chemotherapy. These combination approaches are used to improve treatment.
Several immunotherapies are standard treatments for certain cancers, while others are only offered through clinical trials. Some types of cancer aren’t treatable by current immunotherapies. To extend the benefits of immunotherapy, MD Anderson is leading research to identify new and more effective ways to improve the immune response to cancer.
Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Allison Institute™
Immunotherapy has transformed care for many patients with cancer. However, not all patients benefit. Our goal is to change that.

Featured Articles

Next-generation sequencing and immunotherapy give bladder cancer...

What is the future of cell therapy in cancer treatment?

How beautiful images can advance immunotherapy

Lung cancer survivor grateful for immunotherapy clinical trial

Researcher studies tumor cell interaction to improve...

CAR NK cell therapy now an experimental treatment option for...

What’s new in immunotherapy for prostate cancer?
Which cancers can be treated with immune checkpoint inhibitors?
request an appointment online.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
