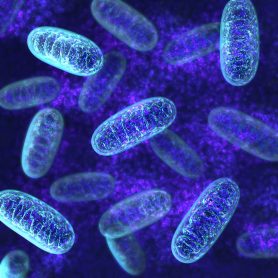
New cancer therapy target found in mitochondria for potential treatment of blood cancers
Study shows how imipridone drugs ONC201 and ONC212 cause cancer cell death
MD Anderson News Release May 02, 2019
A study at The University of Texas MD Anderson Cancer Center identified a new therapeutic target in cancer cells and explains how new anti-cancer drugs called imipridones work by inducing cancer cell death in blood cancers, such as acute myeloid leukemia (AML) and mantle cell lymphoma.
The study revealed a target in mitochondria, called caseinolytic protease P (ClpP), which, upon activation, breaks down proteins within mitochondria, a process known as mitochondrial proteolysis. A new class of anti-cancer agents, called imipridones, were shown to activate ClpP and cause cancer cell death via mitochondrial proteolysis.
The drugs, ONC201 and Onc212, work regardless of whether the common tumor suppressor p53 is present in any form. Findings from the study, led by Michael Andreeff, M.D., Ph.D., professor of Leukemia, and Jo Ishizawa, M.D., Ph.D., assistant professor of Leukemia, were reported in the May 2 online issue of Cancer Cell.
“Despite newly developed targeted agents, the majority of hematologic malignancies and solid tumors are still incurable. This includes essentially all patients with p53 mutations,” said Andreeff. “Therefore, anti-tumor agents with novel mechanisms of action are urgently needed. Our findings support the clinical development of imipridones and other ClpP activators for human cancers.”
Through in vitro and in vivo models, the team demonstrated that knock-out or over-expression of inactivated mutant ClpP induced complete resistance against ONC201 and ONC212, indicating that activation of ClpP is crucial for cell death caused by the drugs. Through extensive crystallography studies, the team identified the exact binding sites and binding patters of the drugs on ClpP and demonstrated how they increased protease activity.
While ONC201 is in early clinical trials for AML and other cancers and its pre-clinical efficacy has been established in numerous cancer models, the direct target behind its success has remained elusive. Pre-clinical toxicology studies have been conducted for ONC212, and it is slated for clinical trials in the near future.
“Deletions or mutations of ClpP have never been reported in primary AML, suggesting that ClpP could be an effective target across the spectrum of molecular and cytogenetic subsets of AML,” said Ishizawa. “Our data indicate that patient samples with the lowest levels of ClpP are less sensitive to ClpP hyperactivation. Thus, levels of ClpP could serve as a biomarker to identify AML patients most likely to respond to this therapy.”
Andreeff added that further studies of larger numbers of patients will be required to establish thresholds of ClpP expressions most likely to predict response.
The study resulted from a strategic alliance and research collaboration between MD Anderson and Oncoceutics, Inc. launched in January 2015 to further develop and identify potential clinical uses for anti-cancer drugs like ONC201 and ONC212.
MD Anderson study team members included: Takenobu Nii, Ph.D.; Ran Zhao; Lauren Heese; Vivian Ruvolo; Yuki Nishida, M.D., Ph.D.; Kensuke Kojima, M.D., Ph.D.; Gautam Borthakur, M.D.; and Hagop Kantarjian, M.D., all of the Department of Leukemia; Eric Davis, M.D.; and Man Chun Ma, Ph.D., of the Department of Lymphoma and Myeloma; Wencai Ma, M.D., Ph.D., of the Department of Bioinformatics & Computational Biology; and Todd Link, Ph.D., of the Department of Genomic Medicine.
Others participating included: Princess Margaret Cancer Center, Toronto; University of Toronto; Saga University, Saga, Japan; and Oncoceutics, Inc., Philadelphia.
The study was funded by the National Institutes of Health (P30CA016672 and P50CA100632), the Leukemia and Lymphoma Society, Canadian Institutes of Health Research, MaRS Innovation, The Ontario Institute for Cancer Research, the Ontario Ministry of Research and Innovation, the Princess Margaret Cancer Centre Foundation, the Ministry of Long Term Health and Planning in the Province of Ontario, the Barbara Baker Chair in Leukemia and Related Diseases, the Paul and Mary Haas Chair in Genetics in Honor of Amanda Marie Whittle, and the NIH Leukemia SPORE Career Enhancement Programs.
The study was also supported by the Myelodysplastic Syndromes and Acute Myeloid Leukemia Moon Shot™, part of MD Anderson’s Moon Shots Program™, a collaborative effort to accelerate the development of scientific discoveries into clinical advances that save patients’ lives. Andreeff serves on the Scientific Advisory Board of, and is a stockholder of Oncoceutics.