MD Anderson Research Highlights for July 13, 2022
Featuring novel targets to treat inflammation and cancer, biomarkers for immunotherapy and targeted therapy response, and a new cell therapy option for osteosarcoma
MD Anderson News Release July 13, 2022
The University of Texas MD Anderson Cancer Center’s Research Highlights provides a glimpse into recent basic, translational and clinical cancer research from MD Anderson experts. Current advances include new targets involved in protecting DNA replication forks and preventing inflammatory responses, a new treatment option for elderly patients with late-stage acute myeloid leukemia, insights into the breast cancer tumor microenvironment, biomarkers of response to targeted and immune therapies, a novel cellular therapy option for osteosarcoma and a new target for inducing ferroptosis in cancer cells.
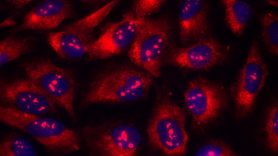
Proteins involved in protecting DNA replication forks prevent inflammatory response
During DNA replication, a structure known as the replication fork coordinates the unwinding and repair of old and new DNA to minimize genomic instability. Stalls at the fork need to be protected to inhibit DNA degradation and to prevent excessive DNA fragments accumulating outside the nucleus, triggering an inflammatory response. Better understanding this process can identify possible treatment targets for inflammation-related diseases and cancer. To investigate the link, researchers led by Ahmed Emam, Ph.D., and Bin Wang, Ph.D., generated cells without Abro1 and FANCD2, two proteins previously shown to be involved in fork protection. Loss of these proteins led to a buildup of cytosolic single-stranded ribosomal DNA, which is detected by the cGAS protein to trigger an immune response. Interestingly, this also led to an increase in P-bodies — granules that form in response to replication stress — showing that Abro1 and FANCD2 normally inhibit their production. This study demonstrates the direct role these proteins play in protecting replication forks and inhibiting an innate immune response, highlighting potential therapeutic targets. Learn more in Nature Cell Biology.
Enasidenib provides benefit for older AML patients with IDH2 mutations
IDH2 mutations occur in 8% to 15% of patients with acute myeloid leukemia (AML), with older patients more likely to have the mutation. In an international Phase III study led by Courtney DiNardo, M.D., researchers compared enasidenib, an oral targeted IDH2 inhibitor, with conventional care regimens (CCR) in patients 60 or older with late-stage, IDH2-mutant AML that had received 2-3 prior therapies. The trial randomized 319 patients to evaluate the primary endpoint of overall survival (OS). Median OS with enasidenib (6.5 months) and CCR (6.2 months) was not significantly different; however, the one-year survival rate was 37.5% with enasidenib and 26.1%. with conventional care. Although enasidenib did not lead to significant improvement in median OS, enasidenib provided meaningful benefits in event-free survival, time to treatment failure, overall response rate, hematologic improvement and transfusion independence in this heavily pretreated and older population of patients with IDH2-mutant AML. This study suggests that enasidenib may be a well-tolerated treatment option for this group of relapsed or refractory patients. Learn more in Blood.
Profiling the breast cancer immune microenvironment suggests PARP inhibitors may enhance anti-tumor immune response
PARP inhibitors, such as talazoparib, can selectively target breast cancer by blocking DNA damage repair in cancer cells. Until now, there hasn’t been a comprehensive look into the tumor immune microenvironment (TiME) to clarify how these PARP inhibitors affect infiltrating immune cells, which would allow for the identification of biomarkers that can harness these pathways. Using pre- and post-treatment samples from 13 patients with BRCA1/2-mutant breast cancer treated with neoadjuvant talazoparib, Tapsi Kumar, Ph.D., Jennifer Litton, M.D., and colleagues profiled the TiME to identify the location of and interactions between immune and tumor cells. While it was a small sample size, they noted phenotypes showing that PARP inhibitor treatment significantly increased infiltrating T cell and cytotoxic T cell density both in the tumor and stroma, suggesting that PARP inhibitors could enhance tumor immunogenicity. This study supports further investigation into combination strategies of PARP inhibitors with immunotherapy in BRCA1/2-mutant breast cancer. Learn more in Clinical Cancer Research.
Melanoma study discovers potential response biomarkers for combination immunotherapy and targeted therapy
In BRAF-mutant melanoma, MEK- and BRAF-targeted therapies can prime the tumor microenvironment to respond to immunotherapy, emphasizing the potential for combination therapies. The Phase III COMBI-i trial evaluated the addition of immune checkpoint inhibitor spartalizumab to BRAF inhibitor dabrafenib and MEK inhibitor trametinib in patients with BRAF V600-mutant melanoma. While the study did not meet its primary endpoint of improved progression-free survival, the combination did achieve an objective response rate of 78%, with 16 patients achieving a complete response. To identify patients most likely to benefit from this combination, researchers led by Hussein A. Tawbi, M.D., Ph.D., analyzed biomarker data from COMBI-i to explore indicators of treatment response. With over 500 patient tissues, this was one of the largest biomarker data sets from a Phase III trial in melanoma. Baseline detectable circulating tumor DNA emerged as a strong independent prognostic variable, consistent with higher tumor burden and lower T cell inflammation signature. A baseline CD4+/CD8+ T-cell ratio above the median also was potentially predictive of improved response to combination therapy, meriting further investigation. Learn more in the Journal for ImmunoTherapy of Cancer.
Novel cell therapy suppresses tumor growth and reduces toxicity in osteosarcoma
Chimeric antigen-targeted (CAR) T cell therapy has not been successful in treating childhood osteosarcoma. This is due in part to the long expansion time required for T-cells prior to infusion, the lack of T cell infiltration into tumors and T cell exhaustion in tumors post infusion. Molecular variations between tumors and within tumors also make it difficult to use a single type of CAR to target these variable antigens. To confront these complications, researchers led by Qing Yang, M.D., Ph.D., Jiemiao Hu, Ph.D., and Shulin Li, Ph.D., tested an alternative cell therapy which uses a membrane-anchored and tumor-targeted interleukin-12 (attIL12) to modify peripheral blood mononuclear cells (PBMCs) from fresh blood. Because there is no need for T cell expansion, treatment with attIL12-PBMCs can be done more quickly than CAR T cell therapy. For both in vivo and in vitro osteosarcoma tumors, attIL12-PBMCs reduced cytokine-associated toxicity and suppressed tumor growth by triggering differentiation of cancer cells into bone-like cells. This study supports further evaluation of attIL12-PBMC cellular therapy in osteosarcoma as a novel treatment option. Learn more in Clinical Cancer Research.
Study discovers novel protein involved in protecting cancer cells from ferroptosis
Ferroptosis is one of several normally occurring pathways that regulate cell death. This process is dependent on iron and protects against the toxic accumulation of lipid peroxides — the oxidized forms of fatty acids. Understanding how cancer may adapt to block ferroptosis can point to new treatment strategies. In a new study led by Shiqi Wu, Chao Mao, Ph.D., and Boyi Gan, Ph.D., researchers discovered a previously unknown role for the mitochondrial enzyme GPD2 in defending against ferroptosis. To discover this connection, researchers performed a metabolic analysis after blocking another well-known ferroptosis defense protein, GPX4, in cancer cells. They clarified the mechanism of action and demonstrated that inhibiting both GPD2 and GPX4 increased ferroptosis in cell lines. Combined deletion of GPD2 and GPX4 in laboratory models also induced ferroptosis and suppressed tumor growth. The results suggest that inhibiting GPD2 may represent a therapeutic strategy to combat ferroptosis defense mechanisms in cancer. Learn more in Proceedings of the National Academy of Sciences.
Study identifies new biomarkers associated with response to Aurora kinase inhibitors
Some subsets of patients with cancer benefit from treatment with Aurora kinase inhibitors, but there are no available biomarkers to predict which will have a favorable response. Researchers led by Haoyan Li, Ph.D., and Di Zhao, Ph.D., sought to identify biomarkers associated with improved response to alisertib, an inhibitor selectively targeting Aurora kinase A (AURKA). Using epigenetic screening and drug sensitivity analyses, they discovered that high expression of the CHD1 protein increases sensitivity to alisertib and demonstrated CHD1’s mechanism of action in this response. Additionally, CHD1 is known to be overexpressed in tumors with deficiency in the PTEN tumor suppressor, highlighting PTEN levels as a potential predictive biomarker for AURKA inhibition. This newly discovered role for CHD1 provides further insight into determining which patients will respond positively to alisertib or other AURKA inhibitors. Learn more in Cancer Research.
In case you missed it
Read below to catch up on recent MD Anderson press releases.