request an appointment online.
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsB-cell Lymphoma
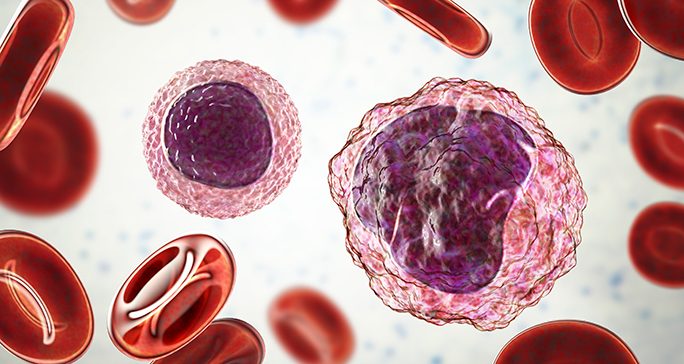
B-cell lymphoma is a type of non-Hodgkin lymphoma that originates in the B-cells. It is the most common type of lymphoma and about 85% of all lymphomas in the United States are B-cell. Common symptoms associated with lymphoma include painless enlargement of one or more lymph node areas, fever, night sweats, and weight loss.
Types of B-cell lymphoma
Diffuse large B-cell lymphoma
Diffuse large B-cell lymphoma (DLBCL) is the most common type of B-cell lymphoma. DLBCL typically affects older people and accounts for one out of three cases of non-Hodgkin lymphoma. This type of B-cell lymphoma usually begins as a mass in a lymph node, but can also form in particular sites such as bone, intestine, the spinal cord or brain.
Standard treatment for DLBCL generally involves months of conventional chemotherapy, and overall cure rates in the last 15 years have been about 70%.
Diffuse large B-cell lymphoma has long been treated as a single disease, but it is now categorized into many different subtypes based on their molecular features. There are two large subtypes: germinal center b-cell (GCB) and activated b-cell (ABC).
Targeted therapies that address the specific molecular features of these DLBCL subtypes are now in clinical trials, and standard therapy may soon depend on subtyping. Based on trials at MD Anderson, CAR T cell therapy is likely to be approved for relapsed or treatment-refractory DLBCL.
Diffuse large B-cell lymphoma can also be categorized based on where it develops. Site-specific forms include:
Primary mediastinal B-cell lymphoma (located within the chest, behind the sternum) has distinctive clinical and molecular features. It is significantly different than other types of DLBCL and, biologically, has more in common with classic Hodgkin lymphoma.
Primary central nervous system lymphoma is rare in general, but is more likely to develop in older populations, as well as those with compromised immune systems. It is almost always DLBCL, particularly the ABC subtype. It can sometimes present in tissues surrounding the eye or spinal cord, but is mostly found throughout the brain and spinal cord.
Follicular lymphoma
The cells of this type of B-cell lymphoma grow in circular structures (follicles), generally within lymph nodes. Follicular lymphomas typically grow slowly, but carry a risk of transformation to the fast-growing GCB-type DLBCL. In some cases, care starts with active surveillance, where the patient is closely monitored for signs of disease progression but is not given any treatments. Most patients are treated initially, however. Standard treatments include targeted therapy without chemotherapy. Around 80% of patients achieve many years of disease-free survival.
Small lymphocytic lymphoma (SLL)/Chronic lymphocytic leukemia (CLL)
The cancer cells in SLL and CLL are identical. The diseases differ based on where these cells are located. SLL cancer cells are mostly in the spleen and lymph nodes, while CLL cancer cells are found mainly in the blood and bone marrow. SLL/CLL predominantly affects older patients and progresses slowly. It can transform into an aggressive disease called Richter’s transformation. Several targeted therapies tested at MD Anderson are now approved or are being evaluated, and can provide years of disease-free survival.
- Learn more about chronic lymphocytic leukemia
Mantle cell lymphoma (MCL)
Mantle cell lymphoma usually affects the lymph nodes, spleen and bone marrow at the time of diagnosis, and is highly variable in its rate of progression. MCL is more likely to affect men and people older than 60. Several targeted therapies tested at MD Anderson are now approved or are being evaluated, and provide chemotherapy-free treatment options for many patients.
Learn more about mantle cell lymphoma
Marginal zone lymphoma
Marginal zone lymphomas are typically slow-growing B-cell lymphomas that comprise 5-10% of lymphoma cases. There are three distinct types, largely based on initial sites of involvement:
MALT lymphoma (extranodal marginal zone B-cell lymphoma or mucosa-associated lymphoid tissue lymphoma)
This is the most common type of MZL. MALT lymphoma originates outside the lymph nodes, often in the stomach. This type of B-cell lymphoma can also start in the skin, lungs or tissues in the mouth and around the eye. Bacterial and viral infections have been shown to cause MALT lymphomas.
Nodal marginal zone B-cell lymphoma
This slow-growing form of MZL is rare and primarily affects older women. It’s typically found in the lymph nodes and occasionally in bone marrow.
Splenic marginal zone B-cell lymphoma
This rare B-cell lymphoma is found almost exclusively in the spleen and bone marrow. It is more common in older men and has been associated with the hepatitis C virus. It is not unusual for an enlarged spleen, common with this type of B-cell lymphoma, to cause fatigue and discomfort.
Burkitt lymphoma
Burkitt lymphoma is a fast-growing B-cell lymphoma that accounts for 1-2% of all lymphomas. Occasionally found in adults, it is much more common in children, especially in boys.
The first-described type of Burkitt lymphoma, endemic to Africa, often presents as a facial tumor and is linked to infection with the Epstein-Barr virus. The variety of Burkitt lymphoma more often seen in the U.S. typically lacks a viral link. It often starts as a large abdominal tumor, less frequently in the testicles or ovaries, and can spread to cerebrospinal fluid.
Burkitt lymphoma is now better classified on the basis of molecular features. It can include some cases that may be confused with DLBCL, but do better with more aggressive chemotherapy.
Waldenstrom macroglobulinemia
Waldenstrom macroglobulinemia is a rare B-cell neoplasm that has features between lymphoma and multiple myeloma. It is most often found in the bone marrow, and typically becomes apparent from symptoms attributable to high blood levels of tumor-produced IgM immunoglobulin, or “macroglobulinemia”.
Learn more about Waldenstrom macroglobulinemia
Hairy cell leukemia
Despite the “leukemia” name, hairy cell leukemia (HCL) is sometimes considered a type of lymphoma, as the cells are B lymphocytes. It is slow-growing, and initial treatment (if any) may include splenectomy for symptoms due to splenic enlargement. Rates of long-term survival or cure are high.
B-cell lymphoma treatment
Treatment for B-cell lymphoma is similar to treatment for other types of non-Hodgkin lymphoma. These options include chemotherapy, radiation therapy, proton therapy, immunotherapy and stem cell transplantation.
Featured Articles

B-cell lymphoma survivor: I experienced marriage and motherhood,...
4 things to know about marginal zone lymphoma

Stage III B cell lymphoma survivor: Go to MD Anderson first

How molecular testing and targeted therapy are changing B-cell...

How I found hope at MD Anderson during non-Hodgkin lymphoma...
Clinical Trials
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.
