request an appointment online.
- Diagnosis & Treatment
- Cancer Types
- Bone Cancer
Get details about our clinical trials that are currently enrolling patients.
View Clinical TrialsIn the United States, more than 3,200 people each year are diagnosed with primary cancer of the bones and joints. These make up 0.2% of all cancers in this country.
In the United States, more than 3,200 people each year are diagnosed with primary cancer of the bones and joints. These make up 0.2% of all cancers in this country.
Bone cancer is a sarcoma (type of cancerous tumor) that starts in the bone. Other cancers may affect the bones, including cancers that metastasize, or spread, from other parts of the body, as well as non-Hodgkin's lymphoma and multiple myeloma. The information on this page focuses on cancers that start in the bones (primary bone cancer).
Bone structure
Bones support and give structure to the body. They usually are hollow. The main parts of the bones are:
Matrix is the outer part of bones. It is made of fiber-like tissue and is covered with a layer of tissue called the periosteaum.
Bone marrow is the soft tissue in the space in hollow bones called the medullary cavity. Cells inside bone marrow include:
- Fat cells
- Red blood cells, white blood cells and platelets
- Fibroblasts, a type of cell that helps build connective tissue
- Plasma, in which blood cells are suspended
Cartilage is at the end of most bones. It is softer than bone, but it is firmer than soft tissue. Cartilage and other tissues, including ligaments, make up joints, which connect some bones.
Bone constantly changes as new bone forms and old bone dissolves. To make new bone, the body deposits calcium into the cartilage. Some of the cartilage stays at the ends of bones to make joints.
Bone cancer types
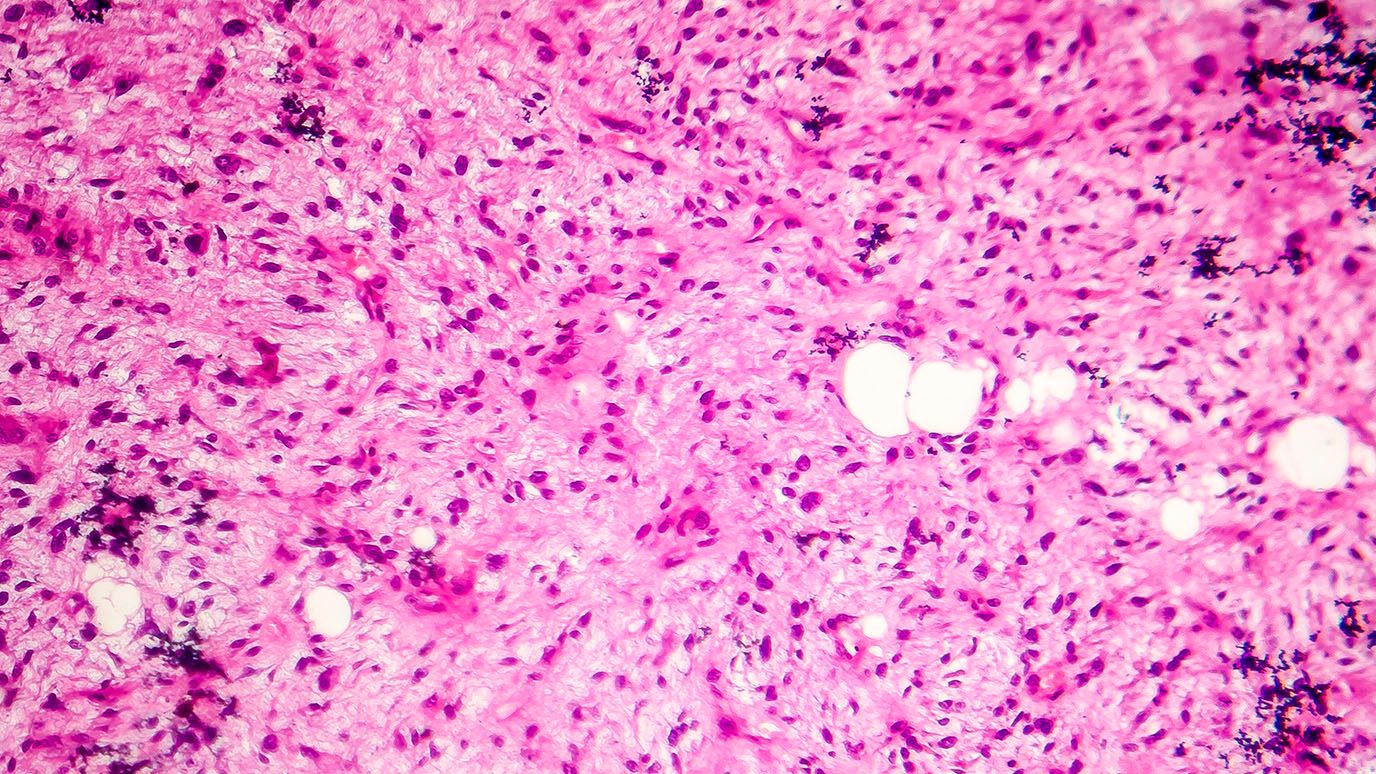
There are several types of bone tumors. They are named according to the area of bone or tissue where they start and the type of cells they contain. Some bone tumors are benign (not cancer), and some are malignant (cancer). Bone cancer also is called sarcoma.
The most commonly found types of primary bone cancer are:
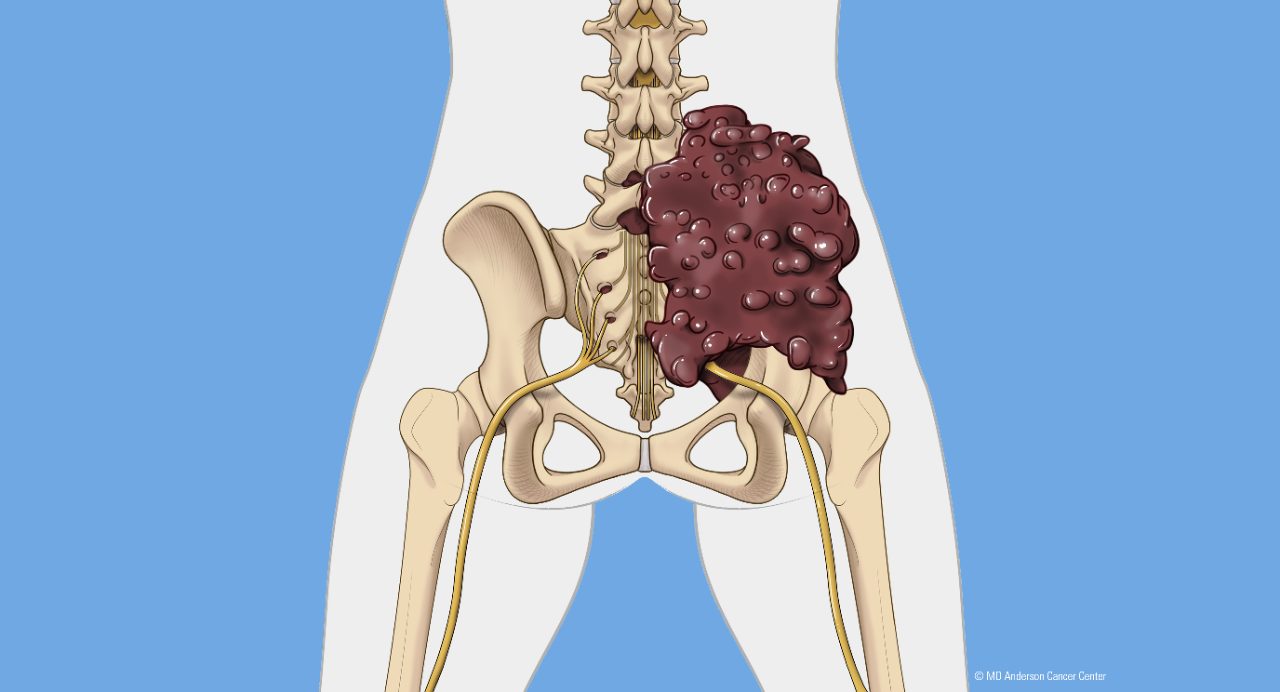
- Osteosarcoma or osteogenic sarcoma is the main type of bone cancer. It occurs most often in children and adolescents, and it accounts for about one-fourth of bone cancer in adults. More males than females get this cancer. About 1,000 people in the United States are diagnosed with osteosarcoma each year. It begins in bone cells, usually in the pelvis, arms or legs, especially the area around the knee.
- Chondrosarcoma is cancer of cartilage cells. More than 40% of adult bone cancer is chondrosarcoma, making it the most prevalent bone cancer in adults. The average age of diagnosis is 51, and 70% of cases are in patients over 40. Chondrosarcoma tends to be diagnosed at an early stage and often is low grade. Many chondrosarcoma tumors are benign (not cancer). Tumors can develop anywhere in the body where there is cartilage, especially the pelvis, leg or arm.
- Ewing's sarcoma is the second most prevalent type of bone cancer in children and adolescents, and the third most often found in adults. It accounts for about 8% of bone cancers in adults. Ewing's sarcoma can start in bones, tissues or organs, especially the pelvis, chest wall, legs or arms.
Less-commonly found types of bone cancer include:
- Chordoma, which is found in 10% of adult bone cancer cases, usually in the spine and base of the skull
- Malignant fibrous histiocytoma/fibrosarcoma, which usually starts in connective tissue
- Fibrosarcoma, which often is benign and found in soft tissue in the leg, arm or jaw
- Secondary (or metastatic) bone cancer is cancer that spreads to the bone from another part of the body. This type of bone cancer is more prevalent than primary bone cancer. For more information about this type of cancer, see the type of primary cancer (where the cancer started).
Bone cancer risk factors
Anything that increases your chance of getting bone cancer is a risk factor. However, having risk factors does not mean you will get bone cancer. In fact, most people who develop bone cancer do not have any risk factors. If you have risk factors, it’s a good idea to discuss them with your health care provider.
Teenagers and young adults are at greatest risk of developing osteosarcoma, a type of bone cancer, because it often is associated with growth spurts.
Some diseases that run in families can slightly increase the risk of bone cancer. These include:
- Li-Fraumeni syndrome
- Rothmund-Thompson syndrome
- Retinoblastoma (an eye cancer of children)
- Multiple osteochondromas
- Genetic counseling may be right for you. Learn more about the risk to you and your family on our genetic
testing page.
Other risk factors for bone cancer include:
- Paget’s disease
- Prior radiation therapy for cancer, especially treatment at a young age or with high doses of radiation
- Bone marrow transplant

MD Anderson is #1 in Cancer Care
Orthopedic oncologist passionate about helping patients...
Understanding chondrosarcoma: symptoms, treatment and...
Why choose MD Anderson for bone cancer treatment?
MD Anderson's Sarcoma Center treats more osteosarcoma, or bone cancer, patients than any other cancer center in the nation. In fact, we are one of the few teams in the world devoted to bone cancer, and our patients have an 80% five-year event-free survival rate.
We bring together a team of experts that includes specialists from many areas to give you personal, customized care. We use specialized therapies and technologies to be sure you receive the most advanced treatment with the least impact on your body.
If possible, it is best to have a biopsy to diagnose bone cancer at the same place you receive treatment. It is essential to go to a specialized cancer center that has experience in osteosarcoma biopsy. If the biopsy is done incorrectly, it may make it more difficult later for the surgeon to remove all of the cancer without having to also remove all or part of the arm or leg. A biopsy that is not done correctly also may cause the cancer to spread.
As one of the world's leading cancer centers, we constantly work to discover new treatments and innovations. We helped pioneer:
- Embolization for localized unresectable giant cell tumor of bone
- Activity of interferon in metastatic giant cell tumor of bone
- Limb-sparing surgery to help save arms and legs
- Targeting a cell receptor known to play a part in the spread of cancer to the bones may enable chemotherapy drugs to be delivered directly to the cells
Being positive is the best medicine you can take.
Maggie Howard
Survivor
Treatment at MD Anderson
Bone cancer (osteosarcoma) is treated in our Sarcoma and Orthopaedic Center.

Clinical Trials
MD Anderson patients have access to clinical trials offering promising new treatments that cannot be found anywhere else.
Becoming Our Patient
Get information on patient appointments, insurance and billing, and directions to and around MD Anderson.
myCancerConnection
Talk to someone who shares your cancer diagnosis and be matched with a survivor.
Prevention & Screening
Many cancers can be prevented with lifestyle changes and regular screening.
Counseling
MD Anderson has licensed social workers to help patients and their loved ones cope with cancer.
Help #EndCancer
Give Now
Donate Blood
Our patients depend on blood and platelet donations.
Shop MD Anderson
Show your support for our mission through branded merchandise.